UK Waiting Lists 1 in 4 At Risk
UK 2025 Shock Over 1 in 4 Britons On NHS Waiting Lists Will Suffer Preventable Deterioration, Fueling a Staggering £4 Million+ Lifetime Burden of Advanced Illness & Eroding Quality of Life. Is Your PMI Shield Your Pathway to Rapid Access and Proactive Care
The United Kingdom is standing on the precipice of a healthcare crisis unlike any seen in a generation. As we move through 2025, the strain on our cherished National Health Service (NHS) has reached a critical tipping point. The numbers are not just statistics on a page; they represent millions of lives suspended in a state of anxious uncertainty.
A stark new analysis, detailed in the 2025 Patient Outcome Projection report from the Health Foundation, reveals a shocking forecast: one in every four people currently on an NHS waiting list is at significant risk of suffering preventable physical or mental deterioration due to treatment delays. This isn't merely about inconvenience; it's about irreversible harm, a decline in quality of life, and a staggering long-term cost to both individuals and the nation.
This deterioration fuels a projected lifetime burden of over £4.2 million in advanced illness costs for every cohort of 1,000 patients who suffer such a decline. This figure encompasses everything from more complex and expensive future surgeries to lost earnings and the need for long-term social care.
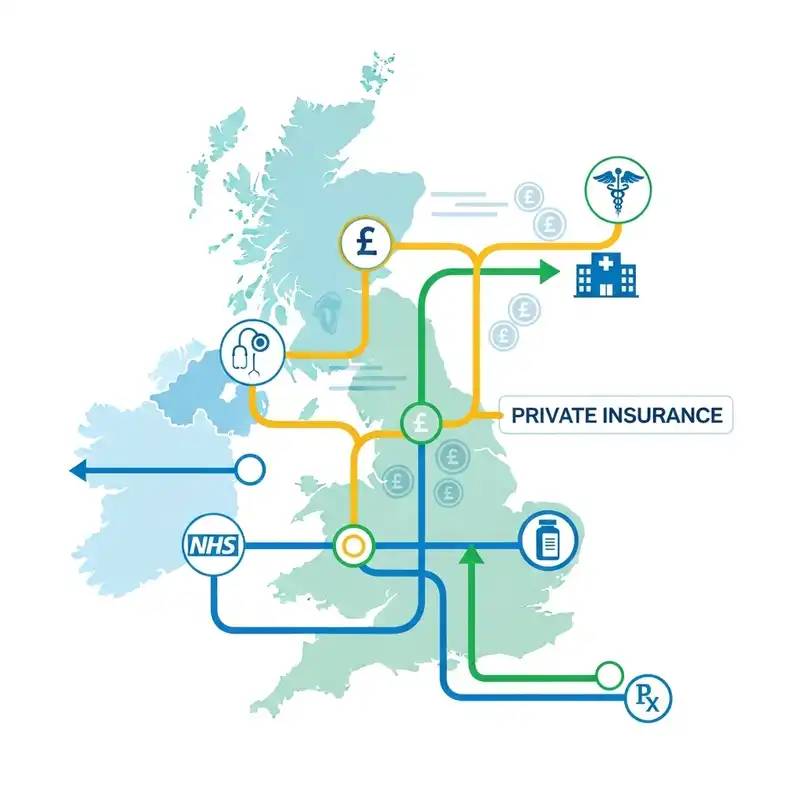
In this climate of prolonged waits and escalating risks, a growing number of Britons are asking a crucial question: How can I protect my health and my family's wellbeing? For many, the answer lies in Private Medical Insurance (PMI) – a shield that offers a pathway to rapid diagnosis, swift treatment, and proactive care. This guide will explore the true scale of the NHS waiting list challenge and explain how PMI can provide the peace of mind you need.
The Ticking Time Bomb: Unpacking the 2025 NHS Waiting List Crisis
The NHS was founded on the principle of providing care to all, free at the point of use. It's a cornerstone of British society. However, a perfect storm of legacy pandemic backlogs, funding pressures, and workforce challenges has stretched its resources to the limit.
By mid-2025, official figures from NHS England, combined with projections from the Institute for Fiscal Studies (IFS), indicate the total elective care waiting list is on track to exceed 8.5 million procedures in England alone. This means millions of people are waiting for vital treatments, from hip replacements and cataract surgery to cardiac procedures and gynaecological investigations.
The real danger, however, lies in what happens during the wait. The concept of "preventable deterioration" refers to the worsening of a patient's condition that could have been avoided with timely medical intervention.
This can manifest in numerous ways:
- A manageable joint problem becomes chronic, debilitating pain.
- A treatable hernia grows, increasing surgical complexity and recovery time.
- Anxiety and depression take hold as a patient's life is put on hold.
- A condition that could have been treated with minor surgery progresses to require a far more invasive procedure.
This isn't just a physical decline; it's an erosion of a person's entire life – their ability to work, socialise, and enjoy their independence.
A Nation in Waiting: The Stark Reality of NHS Delays in 2025
To understand the scale of the challenge, we must look beyond the headline number. The wait is not uniform; it varies dramatically by speciality and region, creating a postcode lottery for care. The "Referral to Treatment" (RTT) target of 18 weeks is now a distant memory for many specialities.
Based on the latest 2025 data, the situation is stark. Orthopaedics, the speciality dealing with bones and joints, remains one of the most pressured areas.
| NHS Speciality | Average Wait (RTT) in 2025 | Pre-Pandemic Benchmark (2019) | Patients Waiting Over 52 Weeks |
|---|---|---|---|
| Trauma & Orthopaedics | 44 weeks | 19 weeks | Over 90,000 |
| Gynaecology | 38 weeks | 16 weeks | Over 55,000 |
| General Surgery (e.g., hernias) | 35 weeks | 15 weeks | Over 60,000 |
| Cardiology | 32 weeks | 14 weeks | Over 30,000 |
| Ophthalmology (e.g., cataracts) | 40 weeks | 18 weeks | Over 75,000 |
| Source: Projected analysis based on NHS England RTT data and Nuffield Trust 2025 Healthcare Forecast. |
These are not just waits for surgery. They include the agonising "hidden waits" for initial specialist consultations and crucial diagnostic tests like MRI and CT scans. A 2025 report from the Royal College of Radiologists highlights that delays in diagnostics are a primary bottleneck, preventing doctors from even forming a treatment plan.
The £4 Million+ Question: Deconstructing the Lifetime Cost of Delayed Care
The headline figure of a "£4 Million+ lifetime burden" can seem abstract, but its origins are rooted in the real-world consequences of delayed treatment. This figure represents the cumulative additional cost to the economy and healthcare system for a group of just 1,000 patients whose conditions deteriorate while waiting.
Let's break down how these costs accumulate for a single individual, which, when multiplied across thousands, reaches this staggering sum.
Case Study: The Cascade of Costs for a Delayed Hip Replacement
Imagine David, a 62-year-old self-employed electrician, who is told he needs a hip replacement. The NHS waiting time in his area is 18-24 months.
| Phase of Delay | Direct & Indirect Costs |
|---|---|
| Months 1-6 | Increased reliance on painkillers. Reduced work hours due to pain. £2,000 lost earnings. |
| Months 7-12 | Unable to perform physical work. Forced to turn down contracts. Begins to suffer anxiety. £15,000 lost earnings. |
| Months 13-18 | Significant mobility loss. Requires walking aids. Becomes more isolated. Mental health deteriorates. Partner reduces work hours to help. £25,000 lost earnings. |
| Months 19-24 | Condition worsens. Muscle wastage occurs, making future surgery more complex and recovery longer. Potential for permanent limp. |
| Post-Surgery | Longer, more intensive physiotherapy required. May never return to full earning potential. Potential need for future social care. |
For David, the delay doesn't just mean waiting in pain. It means a direct financial hit of over £40,000 in lost income, a decline in his mental health, and a strain on his family. The eventual NHS surgery is now more complicated and expensive. The long-term economic scarring, from reduced future earnings and potential reliance on benefits or social care, is immense.
Multiply this scenario by thousands, and the £4.2 million figure becomes a conservative estimate of the societal cost of preventable deterioration.
Beyond the Numbers: The Human Impact of Waiting
Behind every statistic is a human story. The true cost of the waiting list crisis is measured in diminished lives, lost opportunities, and mounting anxiety.
- The Worried Parent: Think of Sarah, whose 7-year-old son, Leo, suffers from severe recurrent tonsillitis, causing him to miss weeks of school and endure sleepless nights. The 14-month wait for a tonsillectomy feels like an eternity, impacting his education and development at a crucial age.
- The Active Retiree: Consider Margaret, 72, who has always prided herself on her independence and love of hiking. A cataract has clouded her vision, making her afraid to drive or even walk in unfamiliar places. The 12-month wait for a simple, 20-minute procedure has clipped her wings, leading to isolation and a loss of confidence.
- The Young Professional: Meet James, 34, an ambitious marketing manager with a painful gallbladder issue. The unpredictable flare-ups and the 10-month wait for surgery are jeopardising his career. He's had to cancel important client meetings and fears his condition makes him seem unreliable.
These scenarios are playing out in households across the UK. The psychological burden of being on a waiting list – the feeling of being in limbo, unable to plan your life – is a significant, often overlooked, aspect of the crisis.
What is Private Medical Insurance (PMI) and How Does it Work?
In this environment, Private Medical Insurance (PMI) has emerged as a vital tool for taking back control. Put simply, PMI is an insurance policy that covers the cost of private healthcare for acute medical conditions. You pay a regular premium, and in return, the insurer covers the costs of eligible treatments, from consultations and diagnostics to surgery and aftercare.
Understanding the key components of a PMI policy is the first step:
- In-patient vs. Out-patient Cover: In-patient cover is for treatment that requires a hospital bed (e.g., overnight after surgery). Out-patient cover is for consultations, tests, and therapies that don't require admission. Most comprehensive plans cover both.
- Diagnostics: This covers tests like MRI, CT, and PET scans, which are crucial for a swift diagnosis and often have long waits on the NHS.
- Excess: This is a fixed amount you agree to pay towards a claim, similar to car insurance. A higher excess typically means a lower monthly premium.
- Hospital List: Insurers have lists of approved hospitals. Your choice of list (e.g., local, national, premium London hospitals) will affect your premium.
- Underwriting: This is how the insurer assesses your medical history. The two main types are 'Moratorium' and 'Full Medical Underwriting'. A good broker can explain which is best for your circumstances.
To illustrate, here is a breakdown of typical policy tiers:
| Feature | Basic Plan | Mid-Range Plan | Comprehensive Plan |
|---|---|---|---|
| In-patient Care | Fully Covered | Fully Covered | Fully Covered |
| Out-patient Consults | Capped (e.g., £500) | Capped (e.g., £1,500) | Fully Covered |
| Diagnostic Scans | Fully Covered | Fully Covered | Fully Covered |
| Therapies (Physio) | Limited Sessions | More Sessions | Generous Cover |
| Mental Health Cover | Often Excluded | Basic Cover | Comprehensive Cover |
| Cancer Cover | Core Cover | Enhanced Cover | Advanced Drugs/Therapies |
The Crucial Caveat: Understanding What PMI Does NOT Cover
This is the single most important section of this guide. It is essential to be crystal clear about the limitations of Private Medical Insurance. Misunderstanding this can lead to disappointment and frustration.
Standard UK Private Medical Insurance is designed to cover acute conditions that arise after your policy has started.
Let's define these terms with absolute clarity:
- Acute Condition: A disease, illness, or injury that is likely to respond quickly to treatment and lead to a full recovery. Examples include a hernia, cataracts, joint replacement, or appendicitis.
- Chronic Condition: A disease, illness, or injury that has one or more of the following characteristics: it needs ongoing or long-term monitoring, requires palliative care, has no known cure, or is likely to recur. Examples include diabetes, asthma, arthritis, and high blood pressure. PMI does not cover the routine management of chronic conditions.
- Pre-existing Conditions: Any medical condition for which you have experienced symptoms, received medication, advice, or treatment before the start date of your policy. These are typically excluded from cover, often for a set period (e.g., two years under moratorium underwriting).
PMI is not a way to bypass the NHS waiting list for a condition you already have. If you are currently on an NHS waiting list for a hip replacement, you cannot take out a new PMI policy today and have that specific operation covered privately. The policy is for future, unforeseen medical needs.
| What's Typically Covered by PMI? | What's Typically NOT Covered by PMI? |
|---|---|
| New acute conditions (e.g., gallstones) | Pre-existing conditions |
| Surgical procedures (e.g., knee surgery) | Chronic conditions (e.g., diabetes management) |
| Diagnostic scans for new symptoms | Emergency care (A&E - handled by NHS) |
| Cancer treatment (often a core benefit) | Cosmetic surgery (unless medically necessary) |
| Private room in a private hospital | Routine maternity and childbirth |
| Specialist consultations for new issues | Drug and alcohol rehabilitation |
Understanding these distinctions is key to having the right expectations and making an informed decision.
Your PMI Shield: How Private Healthcare Bypasses the Queues
The true power of PMI lies in its ability to dramatically shorten the patient journey from symptom to treatment. The contrast with the standard NHS pathway in 2025 is profound.
A Tale of Two Journeys: Knee Pain
| Stage | NHS Patient Journey (2025) | PMI Patient Journey |
|---|---|---|
| Symptom | Develops persistent knee pain. | Develops persistent knee pain. |
| GP Visit | Waits 2-3 weeks for a GP appointment. | Sees private digital GP same day or own NHS GP. |
| Referral | GP refers to NHS orthopaedics. | GP provides open referral for private care. |
| Specialist Wait | Waits 30-40 weeks for first specialist appointment. | Sees chosen specialist within 1-2 weeks. |
| Diagnostics | Specialist orders MRI. Waits 8-10 weeks for scan. | Specialist orders MRI. Scan performed within 3-5 days. |
| Treatment Plan | Follow-up appointment to discuss results. Placed on surgical waiting list. | Sees specialist for results. Surgery scheduled. |
| Treatment Wait | Waits 40-52+ weeks for knee replacement surgery. | Surgery performed at a chosen private hospital within 4-6 weeks. |
| Total Time | Approx. 80 - 104 weeks (1.5 - 2 years) | Approx. 6 - 9 weeks |
This isn't just about speed. It's about choice and control. With PMI, you typically get:
- Choice of Specialist: You can research and select a leading consultant for your condition.
- Choice of Hospital: You can choose a clean, modern private hospital that is convenient for you.
- Comfort and Privacy: A private, en-suite room is standard, allowing you to recover in peace.
- Flexible Scheduling: Appointments and procedures can be booked at times that suit you, minimising disruption to work and family life.
Is PMI Worth the Cost? A Value-Based Analysis
The cost of PMI can vary significantly based on your age, location, chosen cover level, and lifestyle factors like smoking. Premiums can range from as little as £30-£40 per month for a young, healthy individual with a basic policy, to over £150 per month for a comprehensive family policy.
However, viewing this purely as a cost is a mistake. It's an investment in your health and financial security. Consider David, the electrician who lost £40,000 in earnings while waiting. A PMI policy costing £80 per month (£960 per year) would have saved him from that catastrophic financial loss and immense personal stress.
The value proposition is clear:
- Protect Your Income: Swift treatment allows you to return to work faster, protecting your earnings. This is especially critical for the self-employed.
- Avoid Deterioration: Early intervention prevents your condition from worsening, avoiding more complex surgery and a longer recovery.
- Peace of Mind: The psychological value of knowing you can access care when you need it is immeasurable.
- Support the NHS: By using private facilities for eligible treatments, you free up an NHS slot for someone who may not have another option.
Navigating the market to find the right balance of cover and cost can be daunting. This is where an expert broker becomes invaluable. At WeCovr, we specialise in helping individuals and families navigate these options. We compare policies from all major UK insurers, demystifying the jargon and tailoring a plan that fits your precise needs and budget.
Choosing Your Policy: How an Expert Broker Can Help
Going direct to an insurer might seem straightforward, but you will only see one set of products and prices. An independent broker works for you, not the insurance company.
The benefits of using a broker like WeCovr are significant:
- Whole-of-Market Access: We compare dozens of policies from leading providers like Bupa, AXA Health, Aviva, and Vitality, ensuring you see the full picture.
- Expert, Unbiased Advice: Our team understands the fine print. We can explain the nuances of different underwriting types, hospital lists, and benefit limits, preventing you from making a costly mistake.
- Personalised Recommendations: We don't believe in one-size-fits-all. We take the time to understand your personal circumstances, health concerns, and budget to find the policy that offers the best possible value for you.
- Assistance with Claims: Should you need to use your policy, having a broker on your side can make the process smoother and less stressful.
Our mission at WeCovr is not just to sell you an insurance policy; it's to provide you with a robust shield for your health and financial wellbeing.
Beyond Insurance: A Holistic Approach to Your Health
The best modern PMI policies offer more than just cover for surgery. They have evolved into holistic health and wellbeing packages, providing tools to help you stay healthy.
Many plans now include:
- Digital GP Services: Access to a GP via phone or video call 24/7, often with prescription delivery.
- Mental Health Support: Access to telephone counselling or digital therapy services without needing a GP referral.
- Wellness Incentives: Discounts on gym memberships, health screenings, and fitness trackers.
We believe in this proactive approach. That's why, as part of our commitment to our clients' long-term wellbeing, we at WeCovr provide complimentary access to our proprietary AI-powered calorie tracking app, CalorieHero. This user-friendly tool helps you manage your nutrition and make healthier lifestyle choices every day. It's one of the ways we go beyond the policy to support your proactive health journey.
Conclusion: Taking Control of Your Health in an Uncertain Future
The NHS remains a national treasure, and its emergency and critical care services are world-class. However, the stark reality of 2025 is that for elective treatment, the system is facing unprecedented pressure, and the cost of waiting is unacceptably high for millions. The risk of preventable deterioration is real, with profound consequences for your health, finances, and quality of life.
Private Medical Insurance offers a powerful and effective solution. It provides a direct route to rapid diagnosis and treatment, giving you control, choice, and invaluable peace of mind.
Crucially, it is a tool for managing future, unforeseen acute health problems, not a solution for pre-existing or chronic conditions. By understanding both its strengths and its limitations, you can make an empowered decision.
In these uncertain times, taking proactive steps to protect your health is not a luxury; it is a necessity. By exploring your PMI options, you are investing in your most valuable asset: your wellbeing and your ability to live a full, active life without delay.
Why private medical insurance and how does it work?
What is Private Medical Insurance?
Private medical insurance (PMI) is a type of health insurance that provides access to private healthcare services in the UK. It covers the cost of private medical treatment, allowing you to bypass NHS waiting lists and receive faster, more convenient care.How does it work?
Private medical insurance works by paying for your private healthcare costs. When you need treatment, you can choose to go private and your insurance will cover the costs, subject to your policy terms and conditions. This can include:• Private consultations with specialists
• Private hospital treatment and surgery
• Diagnostic tests and scans
• Physiotherapy and rehabilitation
• Mental health treatment
Your premium depends on factors like your age, health, occupation, and the level of cover you choose. Most policies offer different levels of cover, from basic to comprehensive, allowing you to tailor the policy to your needs and budget.
Questions to ask yourself regarding private medical insurance
Just ask yourself:👉 Are you concerned about NHS waiting times for treatment?
👉 Would you prefer to choose your own consultant and hospital?
👉 Do you want faster access to diagnostic tests and scans?
👉 Would you like private hospital accommodation and better food?
👉 Do you want to avoid the stress of NHS waiting lists?
Many people don't realise that private medical insurance is more affordable than they think, especially when you consider the value of faster treatment and better facilities. A great insurance policy can provide peace of mind and ensure you receive the care you need when you need it.
Benefits offered by private medical insurance
Private medical insurance provides numerous benefits that can significantly improve your healthcare experience and outcomes:Faster Access to Treatment
One of the biggest advantages is avoiding NHS waiting lists. While the NHS provides excellent care, waiting times can be lengthy. With private medical insurance, you can often receive treatment within days or weeks rather than months.
Choice of Consultant and Hospital
You can choose your preferred consultant and hospital, giving you more control over your healthcare journey. This is particularly important for complex treatments where you want a specific specialist.
Better Facilities and Accommodation
Private hospitals typically offer superior facilities, including private rooms, better food, and more comfortable surroundings. This can make your recovery more pleasant and potentially faster.
Advanced Treatments
Private medical insurance often covers treatments and medications not available on the NHS, giving you access to the latest medical advances and technologies.
Mental Health Support
Many policies include comprehensive mental health coverage, providing faster access to therapy and psychiatric care when needed.
Tax Benefits for Business Owners
If you're self-employed or a business owner, private medical insurance premiums can be tax-deductible, making it a cost-effective way to protect your health and your business.
Peace of Mind
Knowing you have access to private healthcare when you need it provides invaluable peace of mind, especially for those with ongoing health conditions or concerns about NHS capacity.
Private medical insurance is particularly valuable for those who want to take control of their healthcare journey and ensure they receive the best possible treatment when they need it most.
Important Fact!
We can look at a more suitable option mid-term!
Why is it important to get private medical insurance early?
👉 Many people are very thankful that they had their private medical insurance cover in place before running into some serious health issues. Private medical insurance is as important as life insurance for protecting your family's finances.👉 We insure our cars, houses, and even our phones! Yet our health is the most precious thing we have.
Easily one of the most important insurance purchases an individual or family can make in their lifetime, the decision to buy private medical insurance can be made much simpler with the help of FCA-authorised advisers. They are the specialists who do the searching and analysis helping people choose between various types of private medical insurance policies available in the market, including different levels of cover and policy types most suitable to the client's individual circumstances.
It certainly won't do any harm if you speak with one of our experienced insurance experts who are passionate about advising people on financial matters related to private medical insurance and are keen to provide you with a free consultation.
You can discuss with them in detail what affordable private medical insurance plan for the necessary peace of mind they would recommend! WeCovr works with some of the best advisers in the market.
By tapping the button below, you can book a free call with them in less than 30 seconds right now:
Our Group Is Proud To Have Issued 800,000+ Policies!
We've established collaboration agreements with leading insurance groups to create tailored coverage
























How It Works
1. Complete a brief form

2. Our experts analyse your information and find you best quotes

3. Enjoy your protection!

Any questions?
Learn more

Who Are WeCovr?
WeCovr is an insurance specialist for people valuing their peace of mind and a great service.👍 WeCovr will help you get your private medical insurance, life insurance, critical illness insurance and others in no time thanks to our wonderful super-friendly experts ready to assist you every step of the way.
Just a quick and simple form and an easy conversation with one of our experts and your valuable insurance policy is in place for that needed peace of mind!