TL;DR
When you apply for PMI, the insurer needs to understand your health history to determine what they will and won't cover. This is done through one of two main methods:
Key takeaways
- Emergency Treatment: A&E visits are always handled by the NHS.
- Normal Pregnancy & Childbirth: PMI may cover complications, but not routine maternity care.
- Cosmetic Surgery: Unless it's reconstructive surgery required after an accident or eligible cancer treatment.
- Addiction: Treatment for drug and alcohol abuse.
- Self-inflicted Injuries.
UK 2025 Shock Poor Health Costs Average Brit £2000 Annually
UK 2025 Shock Poor Health Costs Average Brit £2000 Annually
A persistent cough that won't shift. A nagging back pain that makes sitting at your desk a misery. A sudden, worrying symptom that leaves you anxiously waiting for a GP appointment. For millions in the UK, these aren't just minor inconveniences; they are the starting point of a costly and stressful journey.
In 2025, the true price of poor health is becoming alarmingly clear. New analysis reveals a staggering figure: the average British adult is losing over £2,100 a year due to health-related issues. This isn't just about the occasional sick day. It's a toxic cocktail of lost earnings, reduced productivity, and a cascade of hidden, out-of-pocket expenses that quietly drain your bank account. (illustrative estimate)
While we are all rightly proud of our National Health Service, the system is straining under unprecedented pressure. Record waiting lists and regional disparities mean that timely access to care is no longer a guarantee. This delay doesn't just impact your health; it directly impacts your wealth.
In this definitive guide, we will unpack the £2,100 figure, explore the current challenges facing the NHS, and explain how Private Medical Insurance (PMI) is evolving from a 'luxury perk' into an essential tool for protecting both your physical and financial wellbeing.
The £2,100 Hole in Your Pocket: Unpacking the Financial Burden of Poor Health
That headline figure might seem steep, but when you break down the components, the reality for many is even starker. The cost of ill health extends far beyond the salary you lose from a day off work. It's a creeping expense that manifests in multiple, often overlooked, ways.
The Double Whammy: Lost Earnings and "Presenteeism"
Sickness absence is at a record high. 8 million people** are now economically inactive due to long-term sickness, a sharp increase over the last five years.
For an employee on the average UK salary, a week off work can mean a significant loss in pay, especially for those without a generous company sick pay scheme. For the UK's 4.2 million self-employed workers, the equation is brutal: if you don't work, you don't get paid.
But the problem runs deeper than simple absenteeism. "Presenteeism"—the act of working while you are unwell—is a silent productivity killer. When you're battling a migraine or struggling with joint pain, your focus, creativity, and efficiency plummet. You're physically present, but your output is a fraction of its normal level, impacting your performance, potential for bonuses, or ability to take on more lucrative projects.
The Hidden Out-of-Pocket Expenses We All Ignore
Beyond lost income, a raft of direct costs quickly accumulates. These are the expenses that rarely feature in our monthly budgets but can collectively amount to hundreds, if not thousands, of pounds a year.
| Expense Category | Description & Example | Estimated Annual Cost Range |
|---|---|---|
| Prescriptions & Remedies | NHS prescription charges in England (£9.90 per item in 2025), plus over-the-counter medication (painkillers, cold remedies, supplements). | £50 - £250+ |
| Travel & Parking | Fuel, parking charges (£3-£5 per hour at many hospitals), or public transport fares for GP, hospital, and specialist appointments. | £100 - £400+ |
| Private Diagnostics | Paying for a private MRI, ultrasound, or consultation to bypass long NHS waits for a diagnosis. | £300 - £1,500+ (per instance) |
| Specialist Equipment | Ergonomic chairs for back pain, blood pressure monitors, physiotherapy aids, or minor home adjustments. | £75 - £500+ |
| Dependant Care | Arranging extra childcare or eldercare to cover you while you attend appointments or recover from a procedure. | £50 - £300+ |
| Wellness & Therapies | Paying for services not readily available on the NHS, like physiotherapy, osteopathy, or private counselling. | £200 - £1,000+ |
As the table shows, a single episode of illness requiring diagnostics and follow-up care can easily push you towards the £2,000 mark before you even account for any lost income.
The Mental Toll's Financial Ripple Effect
The link between physical and mental health is undeniable. The stress of waiting for a diagnosis, the anxiety of being in pain, and the worry about financial instability can be crippling. According to Mind, 1 in 4 people will experience a mental health problem each year.
When NHS talking therapies have waiting lists stretching for months, many feel forced to seek private help, with counselling sessions costing between £50 and £150. This mental strain also impairs financial decision-making and further erodes productivity, creating a vicious cycle of poor health and financial distress.
The UK's Health Crossroads: Navigating NHS Pressures in 2026
The NHS remains one of the UK's most cherished institutions, providing exceptional care to millions. However, it's crucial for every individual and family to understand the immense pressures it currently faces. Acknowledging these challenges is the first step in planning how to safeguard your own health.
The Reality of Record-Breaking Waiting Lists
The defining health story of the mid-2020s is the NHS waiting list for elective treatment in England. By mid-2025, the list has stabilised but remains at a historically high level, with over 7.7 million treatment pathways yet to be completed.
This isn't just a number; it represents millions of people living with pain, discomfort, and uncertainty. The delay between a GP referral and actual treatment can have profound consequences.
Average NHS Waiting Times for Common Procedures (Referral to Treatment, Q2 2025)
| Procedure | Average Waiting Time | Potential Impact of Delay |
|---|---|---|
| Hip Replacement | 45 weeks | Worsening pain, reduced mobility, reliance on painkillers. |
| Knee Replacement | 48 weeks | Joint deterioration, muscle weakness, loss of independence. |
| Cataract Surgery | 38 weeks | Progressive vision loss, increased risk of falls, inability to drive. |
| Hernia Repair | 35 weeks | Increased pain, risk of strangulation requiring emergency surgery. |
| Gynaecology (non-urgent) | 42 weeks | Ongoing pain, anxiety, potential for condition to worsen. |
Source: NHS England Statistics, internal analysis for 2025 trends.
These are averages. In some regions and for some specialities, waits can exceed a year, turning a manageable condition into a life-altering one.
The "Postcode Lottery" is More Prevalent Than Ever
Where you live in the UK can significantly determine the quality and speed of healthcare you receive. Data from organisations like The King's Fund and the Nuffield Trust consistently highlights stark regional disparities.
For example, the waiting time for a key diagnostic test like an endoscopy might be 6 weeks in one NHS Trust but over 20 weeks in another. This "postcode lottery" means your recovery timeline and ability to return to work can depend entirely on your address.
The Domino Effect: How Delays Impact Diagnosis and Outcomes
The most dangerous aspect of long waits is the delay in diagnosis. A symptom that is quickly investigated can often be treated simply and effectively. Left for months, it can evolve. A small, benign polyp could become cancerous. A minor joint issue could lead to irreversible arthritis.
This clinical risk has a direct financial translation. A condition that might have been solved with a minor, day-case procedure could, after a long wait, require major surgery, a longer hospital stay, and a much more protracted recovery period—all of which translates to more time off work and higher personal costs.
What is Private Medical Insurance (PMI) and How Does It Actually Work?
Faced with these challenges, a growing number of people are turning to Private Medical Insurance (PMI) for a greater sense of control and security. But what exactly is it?
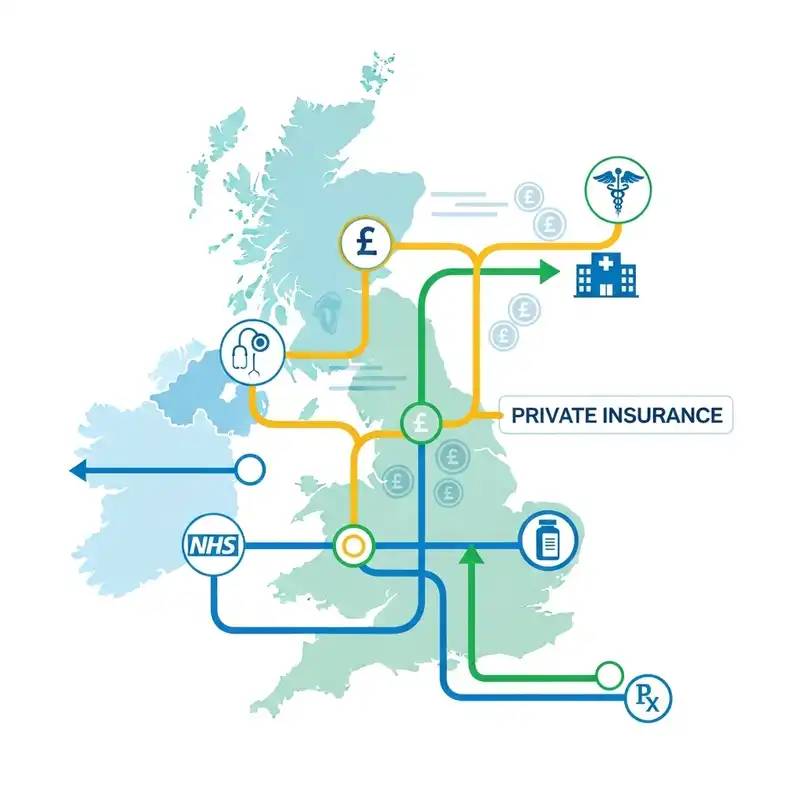
In simple terms, PMI is an insurance policy that covers the cost of private medical treatment for specific types of health conditions. You pay a regular premium (monthly or annually), and in return, the insurer pays for your eligible private healthcare, from specialist consultations and diagnostic scans to surgery and hospital stays.
It's designed to work alongside the NHS, not replace it. The NHS remains your port of call for accidents and emergencies, GP services, and the management of long-term, chronic illnesses. PMI steps in to provide faster access and more choice for treatable, short-term conditions.
The Most Important Rule: Acute vs. Chronic Conditions
Understanding this distinction is absolutely critical to understanding PMI. If you take one thing away from this guide, let it be this:
Standard UK Private Medical Insurance is designed to cover acute conditions. It does NOT cover chronic or pre-existing conditions.
- An Acute Condition: A disease, illness, or injury that is likely to respond quickly to treatment and lead to a full recovery. It has a clear start and end. Examples include cataracts, a hernia, joint pain requiring replacement, or appendicitis.
- A Chronic Condition: A disease, illness, or injury that is long-lasting. It has one or more of the following characteristics: it needs ongoing monitoring, it has no known cure, it's likely to recur, or it requires long-term management. Examples include diabetes, asthma, high blood pressure, and arthritis.
PMI gives you a way to fix a problem that arises after you take out the policy. It is not a way to get private treatment for a condition you already have or one that requires lifelong management.
A Quick Look at Underwriting: How Insurers Assess You
When you apply for PMI, the insurer needs to understand your health history to determine what they will and won't cover. This is done through one of two main methods:
| Underwriting Type | How It Works | Pros | Cons |
|---|---|---|---|
| Moratorium | No initial medical questionnaire. The policy automatically excludes any condition you've had symptoms, treatment, or advice for in the last 5 years. This exclusion can be lifted if you remain symptom-free for a continuous 2-year period after your policy starts. | Quick and simple to set up. Pre-existing conditions can potentially become eligible for cover in the future. | "Wait and see" approach. You may not be 100% certain what's covered until you make a claim. |
| Full Medical Underwriting (FMU) | You complete a detailed health questionnaire. The insurer reviews your medical history and lists any specific conditions that will be permanently excluded from cover from day one. | Complete clarity. You know exactly what is and isn't covered from the start. | The application process is longer. Exclusions are typically permanent. |
How PMI Protects Your Wallet and Wellbeing in 2026
Now, let's connect the dots. How does a PMI policy directly combat the £2,100+ annual cost of poor health and the stress of NHS waits?
Bypass the Queues, Stop the Clock on Lost Earnings
This is the most immediate and powerful benefit of PMI. Let's revisit our earlier waiting list table, but this time with PMI.
- Real-World Scenario: Mark, a 45-year-old self-employed builder, develops severe hip pain. His GP suspects he needs a hip replacement.
- NHS Path: He is referred to a specialist. The wait for an initial consultation is 16 weeks. The wait for an MRI scan is another 10 weeks. The final wait for surgery is 45 weeks. Total time: Over 18 months. During this time, Mark is unable to work effectively, relying on painkillers and losing significant income.
- PMI Path: Mark gets a GP referral and calls his insurer. He sees a private specialist within a week. He has an MRI scan three days later. Surgery is scheduled for two weeks after that. Total time: Under one month. He is back on his feet and earning again in a fraction of the time.
For Mark, the PMI policy didn't just pay for the surgery; it protected over a year of his income, saving him tens of thousands of pounds.
Covering the Eye-Watering Costs of Private Treatment
Choosing to "go private" without insurance is an option, but it's an expensive one. PMI shields you from these significant, one-off costs.
| Procedure | Typical Private Cost (2025) | Covered by a Comprehensive PMI Policy? |
|---|---|---|
| MRI Scan (one part) | £450 - £800 | Yes |
| Knee Arthroscopy | £4,000 - £6,000 | Yes |
| Cataract Surgery (per eye) | £2,500 - £4,000 | Yes |
| Hernia Repair | £3,000 - £5,000 | Yes |
| Hip Replacement | £13,000 - £16,000 | Yes |
A PMI policy with a monthly premium of, say, £70 suddenly looks like exceptional value when faced with a single bill for £15,000. (illustrative estimate)
More Than Just a Hospital Bed: The Added Value of Modern PMI
Today's PMI policies offer a suite of benefits designed to keep you healthy and provide support when you need it most. These often include:
- 24/7 Digital GP: Get a virtual GP appointment via phone or video call, often within hours. Perfect for getting quick advice, prescriptions, or a referral without waiting weeks to see your local GP.
- Mental Health Support: Most leading policies now include access to telephone counselling or a set number of face-to-face therapy sessions, helping you tackle stress, anxiety, and other issues before they escalate.
- Wellness Programmes: Many insurers, like Vitality and Aviva, offer rewards and discounts for staying active, including reduced gym memberships, fitness tracker deals, and healthy food discounts.
At WeCovr, we believe in proactive health management beyond what a standard policy provides. That's why our clients not only get a meticulously chosen insurance plan but also receive complimentary access to our proprietary AI-powered calorie tracking app, CalorieHero. It's our way of helping you invest in your day-to-day wellness, supporting the very foundation of good health.
Demystifying Your Policy: What's Included and What's Not?
A PMI policy document can be complex. To avoid surprises when you need to make a claim, it's essential to understand the structure of cover. Policies are typically built from a core foundation with optional extras you can add on.
Standard Inclusions in a Core Policy
Almost all PMI policies will cover the costs associated with in-patient and day-patient care. This means:
- Hospital charges: The cost of your room, nursing care, and food.
- Specialist fees: Bills from the surgeon, anaesthetist, and consulting physicians.
- Diagnostics: Scans (MRI, CT, PET) and tests carried out while you are admitted to hospital.
- Cancer Cover: This is a cornerstone of modern PMI. Most policies offer extensive cover for the diagnosis and treatment of cancer, including surgery, chemotherapy, and radiotherapy. The level of cover can vary, so it's a key area to compare.
Common Optional Extras to Consider
To create a more comprehensive policy, you can choose to add benefits like:
- Out-patient Cover: This is the most popular add-on. It covers diagnostic tests and specialist consultations that do not require a hospital bed. Without this, you would rely on the NHS for your diagnosis journey and only use PMI for the treatment itself.
- Therapies Cover: Pays for a set number of sessions with a physiotherapist, osteopath, or chiropractor.
- Mental Health Cover: Extends the basic mental health support to cover more extensive consultations with psychiatrists and more therapy sessions.
- Dental and Optical Cover: Provides a contribution towards routine check-ups, dental treatments, and the cost of glasses or contact lenses.
Standard Exclusions You MUST Be Aware Of
Every insurance policy has exclusions. For PMI, these are clear and consistent across the market. As well as the crucial exclusion of chronic and pre-existing conditions, you will generally not be covered for:
- Emergency Treatment: A&E visits are always handled by the NHS.
- Normal Pregnancy & Childbirth: PMI may cover complications, but not routine maternity care.
- Cosmetic Surgery: Unless it's reconstructive surgery required after an accident or eligible cancer treatment.
- Addiction: Treatment for drug and alcohol abuse.
- Self-inflicted Injuries.
Choosing the Right PMI: A Practical Guide
The UK health insurance market is competitive, with a wide range of products available. Finding the right one requires balancing cost with the level of cover you need.
Key Levers That Affect Your Policy and Premium
When building your quote, you will make choices in these four key areas:
- Level of Cover: Do you want a basic 'core' policy that just covers in-patient treatment, or a comprehensive plan with out-patient, therapies, and mental health cover?
- Hospital List: Insurers have tiered hospital lists. A plan that only gives you access to local or regional hospitals will be cheaper than one that includes the premium private hospitals in Central London.
- Excess: This is the amount you agree to pay towards the first claim you make in a policy year. Choosing a higher excess (e.g., £500 instead of £100) will significantly lower your monthly premium.
- The '6-Week Wait' Option: Some policies offer a reduced premium if you agree to use the NHS if the waiting list for your required treatment is less than six weeks. If it's longer, your private cover kicks in. This can be a good cost-saving measure.
The Smart Choice: Why Use an Expert Broker Like WeCovr?
Trying to compare policies from Bupa, AXA Health, Vitality, Aviva, and The Exeter on your own is a recipe for confusion. Each has different definitions, cancer cover promises, and hospital lists. It's not a like-for-like comparison.
This is where an independent, expert broker like WeCovr is indispensable.
Our role is to be your expert guide. We take the time to understand your personal circumstances, health priorities, and budget. Then, we do the hard work for you. We search the entire market and present you with clear, easy-to-understand options from all the UK's leading insurers. We highlight the crucial differences and help you find the policy that offers the best possible value for your specific needs. Our advice is impartial, our service is free, and our goal is to give you confidence and peace of mind.
Frequently Asked Questions (FAQ)
Can I get PMI if I have a pre-existing condition?
You can still get a policy, but it will not cover your pre-existing conditions from the start. However, if you choose a 'moratorium' underwriting policy, that condition could become eligible for cover if you go for a continuous two-year period without needing any treatment, medication, or advice for it after your policy begins.
Is PMI worth it if I'm young and healthy?
Absolutely. Taking out a policy when you are young and healthy means your premiums will be at their lowest. You are insuring against the unexpected future. An accident or a sudden diagnosis can happen at any age, and being prepared provides immense security. It's about protecting your health and your future earnings potential.
Do I still need the NHS if I have PMI?
Yes, 100%. PMI and the NHS work together. The NHS provides all your emergency care, GP services (though PMI can supplement this with digital GPs), and management of any long-term chronic conditions. PMI is your key to getting fast-tracked treatment for new, acute conditions.
How much does PMI cost in 2026?
Costs vary widely based on age, location, level of cover, and excess. As a rough guide, a healthy 30-year-old might pay £40-£60 per month for a comprehensive policy. A 50-year-old might pay £80-£120 per month for similar cover. Family policies and plans with premium hospital access will cost more. The best way to find out is to get a tailored quote. (illustrative estimate)
Does my company's PMI policy cover my family?
This depends entirely on the scheme your employer has negotiated. Some schemes cover the employee only, with an option to add family members at your own cost. More generous schemes might cover your partner and even your children. It's crucial to check your policy documents or speak to your HR department.
Taking Control of Your Health and Finances in 2026
The evidence is clear. In 2025, the cost of poor health is no longer a vague concept; it's a tangible, calculable risk to your financial stability, costing the average person over £2,100 a year in lost productivity and hidden expenses.
While the NHS remains a pillar of our society, relying on it solely for all your healthcare needs in the current climate means accepting the possibility of long, anxious waits that can worsen both your health and your bank balance.
Private Medical Insurance offers a powerful, proactive solution. It is a tool to safeguard your income, ensure your family's wellbeing, and give you the peace of mind that comes from knowing you can access high-quality medical care precisely when you need it most. It's an investment not just in treating illness, but in preserving your quality of life.
Making the right choice can feel complex, but you don't have to do it alone. The team of expert advisors at WeCovr is here to provide the clarity and guidance you need. Let us help you take the first step towards a healthier and more financially secure future.
Sources
- NHS England: Waiting times and referral-to-treatment statistics.
- Office for National Statistics (ONS): Health, mortality, and workforce data.
- NICE: Clinical guidance and technology appraisals.
- Care Quality Commission (CQC): Provider quality and inspection reports.
- UK Health Security Agency (UKHSA): Public health surveillance reports.
- Association of British Insurers (ABI): Health and protection market publications.