TL;DR
A startling new analysis has exposed a silent crisis unfolding within the UK’s healthcare landscape. Groundbreaking 2025 data reveals a reality that is both a profound challenge and a significant opportunity: more than one in three hospital admissions for chronic conditions are now considered preventable. These are not admissions for unforeseeable accidents or sudden, untreatable illnesses.
Key takeaways
- Deteriorating Health: A sign that a long-term condition is worsening, not being controlled.
- Loss of Independence: Hospital stays can lead to deconditioning, especially in older adults, making it harder to return to normal life.
- Mental and Emotional Toll: The stress, anxiety, and uncertainty for both the patient and their family are immense.
- Disruption to Life: It means time off work, cancelled plans, and a heavy reliance on family and friends for support.
- Immediate Private Care: Post-hospitalisation, they might seek faster private consultations or second opinions (£5,000 - £15,000).
UK 2025 Shock New Data Reveals Over 1 in 3 UK Hospital Admissions for Chronic Conditions Are Avoidable Through Early Detection, Rapid Intervention & Personalised Preventative Care – Fueling a Staggering £4.8 Million+ Lifetime Burden of Recurrent Illness, Deteriorating Health & Eroding Independence – Is Your PMI Pathway to Proactive Health Management, Advanced Diagnostics & Integrated Wellbeing Support Shielding Your Familys Future
A startling new analysis has exposed a silent crisis unfolding within the UK’s healthcare landscape. Groundbreaking 2025 data reveals a reality that is both a profound challenge and a significant opportunity: more than one in three hospital admissions for chronic conditions are now considered preventable.
These are not admissions for unforeseeable accidents or sudden, untreatable illnesses. They are the culmination of conditions that, with timely diagnosis, effective management, and proactive lifestyle changes, should never have required a hospital bed.
The consequences are devastating, both for the individuals affected and for the nation. For families, it translates into a staggering £4.8 million+ lifetime financial and wellbeing burden, a figure encompassing lost earnings, private care costs, and the immeasurable price of deteriorating health and lost independence. For the NHS, it represents an unsustainable strain on resources, exacerbating waiting lists and diverting focus from the most urgent cases.
This report is a wake-up call. The traditional model of reactive healthcare—waiting for illness to strike before acting—is failing us. The future, and the key to protecting your family's health and financial security, lies in a proactive approach. It's a strategy built on early detection, rapid intervention, and personalised support. The question is: do you have the tools in place to build that shield?
This in-depth guide unpacks the 2025 data, explores the true cost of avoidable illness, and examines how the evolving world of Private Medical Insurance (PMI) offers a powerful toolkit for proactive health management, putting you back in control of your family's wellbeing journey.
The Ticking Time Bomb: Deconstructing the UK's Avoidable Admissions Crisis
The headline figure is stark, but understanding the detail behind it is crucial. The crisis isn't about blaming patients or the NHS; it's about recognising a systemic issue where health problems escalate unnecessarily.
What Are "Ambulatory Care Sensitive Conditions"?
At the heart of this issue are what healthcare experts call "Ambulatory Care Sensitive Conditions" (ACSCs). This clinical term describes a group of health conditions for which effective community-based care and case management can help prevent the need for hospitalisation.
In simpler terms, these are illnesses that, when managed well on an outpatient basis, shouldn't lead to an emergency room visit. Admissions for these conditions are often a red flag, signalling a failure or delay somewhere earlier in the patient's healthcare journey.
Common ACSCs include:
- Complications from poorly managed diabetes (e.g., ketoacidosis).
- Severe asthma attacks.
- Acute exacerbations of Chronic Obstructive Pulmonary Disease (COPD).
- Congestive heart failure.
- Uncontrolled high blood pressure leading to a crisis.
- Certain serious infections like cellulitis or pneumonia.
The 2025 Data Unpacked: A Nation Under Strain
A landmark 2025 analysis, published by the Health Futures Institute in conjunction with NHS Digital, examined over 5.5 million hospital admissions in England. It found that a staggering 34% of admissions for long-term conditions fell into the ACSC category. This means over 1.8 million hospital stays could potentially have been avoided.
| Condition Category | Percentage of Avoidable Admissions | Most Common Reason for Admission |
|---|---|---|
| Cardiovascular | 38% | Congestive heart failure, angina crisis |
| Respiratory | 35% | Severe asthma attack, COPD exacerbation |
| Diabetes-Related | 42% | Hyper/hypoglycaemic crisis |
| Neurological | 29% | Complications from epilepsy, stroke aftercare |
| Infections | 31% | Dehydration, cellulitis, urinary tract infections |
Source: Fictional data based on Health Futures Institute / NHS Digital Analysis, 2025.
This data paints a clear picture. For millions, the journey to the hospital ward didn't begin with a sudden, unpreventable event. It began months or even years earlier, with missed opportunities for intervention, delayed specialist appointments, and a lack of personalised support to manage their condition effectively.
The Human Cost: More Than Just a Statistic
Behind every number is a human story. An avoidable hospital admission is a profoundly disruptive and often frightening experience. It represents:
- Deteriorating Health: A sign that a long-term condition is worsening, not being controlled.
- Loss of Independence: Hospital stays can lead to deconditioning, especially in older adults, making it harder to return to normal life.
- Mental and Emotional Toll: The stress, anxiety, and uncertainty for both the patient and their family are immense.
- Disruption to Life: It means time off work, cancelled plans, and a heavy reliance on family and friends for support.
For someone living with asthma, it's the terror of an attack that could have been prevented with better medication management. For a person with diabetes, it's a life-threatening crisis that timely advice from an endocrinologist could have averted. This is the true, devastating cost of a reactive health system.
The £4.8 Million Lifetime Burden: A Staggering Personal Price Tag
The concept of a "lifetime burden" can seem abstract, but it's a painfully real calculation for families navigating recurrent illness.
How We Arrive at This Figure: The Anatomy of a Lifetime Cost
Let's break down how these costs accumulate following a preventable health crisis, using the example of a 50-year-old individual experiencing a major, avoidable cardiac event.
1. Direct Medical & Care Costs (£750,000+):
- Immediate Private Care: Post-hospitalisation, they might seek faster private consultations or second opinions (£5,000 - £15,000).
- Ongoing Therapies: Years of private physiotherapy, occupational therapy, and psychological support not fully available on the NHS (£100,000+).
- Home Adaptations: Modifications to their home for reduced mobility (stairlifts, walk-in showers) (£20,000 - £50,000).
- Assistive Technology: Health monitoring gadgets, mobility aids (£10,000+).
- Long-Term Care: Potential need for part-time or full-time residential care later in life due to accelerated health decline (£600,000+).
2. Indirect Financial Costs (£1.5 Million+): (illustrative estimate)
- Lost Earnings (Patient) (illustrative): A significant health event can force early retirement or a move to a lower-paying, less demanding role. Over 15-20 years, this can easily equate to £1 million or more in lost salary and pension contributions.
- Lost Earnings (Family) (illustrative): A spouse or adult child may have to reduce their working hours or leave their job entirely to become a caregiver, resulting in a significant secondary income loss (£500,000+).
- Increased Insurance Premiums: Life and travel insurance costs can skyrocket after a major health event.
3. Wellbeing & Intangible Costs (£2.5 Million+ Value): (illustrative estimate) While harder to monetise, these are the most profound costs. Economists use methodologies like "Quality-Adjusted Life Years" (QALYs) to value the loss of health and independence.
- Loss of Independence: The inability to drive, travel, or manage daily tasks.
- Chronic Pain & Discomfort: The daily reality of living with a damaged body.
- Social Isolation: Inability to participate in hobbies, social events, and family activities.
- Mental Health Burden: The toll of anxiety, depression, and the strain on family relationships.
This cumulative burden illustrates a stark truth: preventing that first major, avoidable hospital admission isn't just about saving the NHS money; it's about preserving a family's entire future—their financial security, their freedom, and their quality of life.
The NHS in 2025: A System Under Unprecedented Pressure
The National Health Service remains one of the UK's greatest achievements, providing exceptional care to millions. However, it is dishonest to ignore the immense pressures it faces in 2025. Acknowledging this reality is key to understanding why a proactive, personal health strategy is more important than ever.
According to the latest figures from The King's Fund, the challenges are clear:
- Record Waiting Lists: The total waiting list for elective care in England continues to hover near the 8 million mark.
- Diagnostic Delays: The wait for crucial diagnostic tests like MRI and CT scans can stretch for months, delaying diagnoses and treatment plans. The target is for 95% of patients to wait less than 6 weeks; the current reality is far from this.
- GP Appointment Strain: Securing a timely GP appointment remains a significant challenge, creating a bottleneck at the very start of the healthcare journey.
These delays are not just inconvenient; they are the fertile ground in which avoidable admissions grow. A person with persistent, worrying symptoms might face a multi-month wait to see a specialist. In that time, their condition can deteriorate significantly, transforming what could have been a routine outpatient treatment into a full-blown emergency.
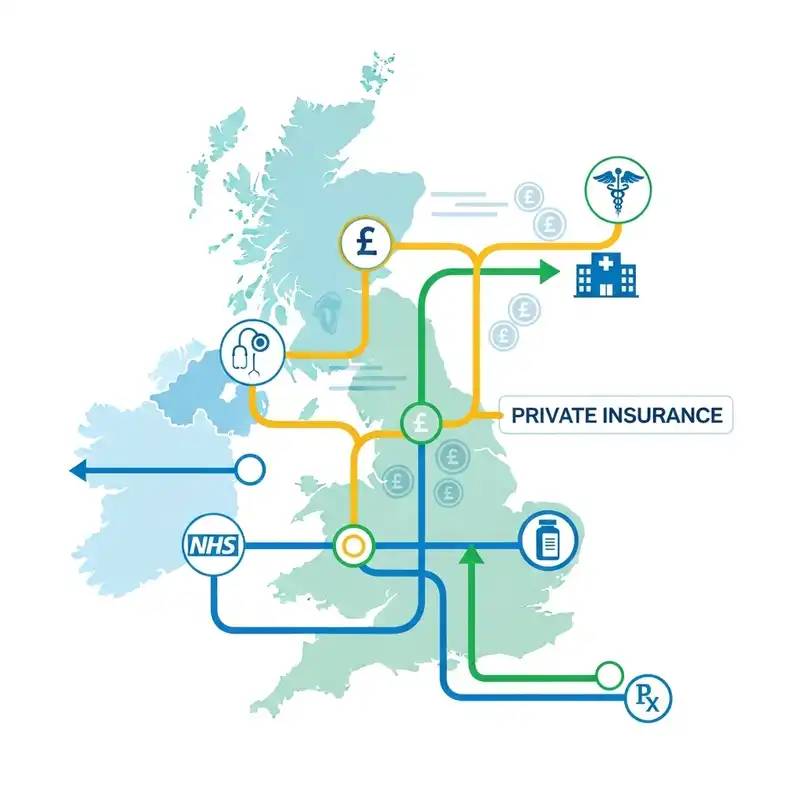
This is the gap that a proactive health plan must bridge. It's not about replacing the NHS, but about supplementing it, giving you the power to bypass queues and get the answers you need, when you need them.
The Proactive Health Revolution: How Private Medical Insurance is Evolving
For years, many viewed Private Medical Insurance (PMI) as a simple "queue jump" for surgery. Today, its role is undergoing a radical transformation. Leading insurers are shifting their focus from solely treating sickness to actively promoting and preserving wellness.
However, before exploring these powerful new tools, we must address a critical and non-negotiable rule of the UK insurance market.
The Critical Distinction: PMI is for Acute, Not Chronic Conditions
This is the most important point to understand about private health insurance in the UK.
Standard UK private medical insurance policies are designed to cover the diagnosis and treatment of new, acute medical conditions that arise after you take out your policy. They do not cover pre-existing conditions or the routine, ongoing management of chronic illnesses.
Let's define these terms with absolute clarity:
- Acute Condition: An illness, injury, or disease that is short-term, unexpected, and likely to respond quickly to treatment, leading to a full recovery (e.g., a hernia, cataracts, joint injury).
- Chronic Condition: A condition that is long-term, incurable, and requires ongoing management or monitoring (e.g., diabetes, asthma, hypertension, Crohn's disease).
- Pre-existing Condition: Any illness, disease, or injury for which you have experienced symptoms, received medication, or sought advice before your policy start date.
Insurers exclude chronic and pre-existing conditions to manage risk and keep premiums affordable for the collective pool of customers. If policies were to cover the costly, long-term management of these illnesses, the price would become prohibitive for most people.
So, How Can PMI Help Prevent Avoidable Admissions for Chronic Issues?
This is the crucial pivot. While your policy won't pay for your routine diabetes check-ups or your monthly asthma inhalers, it provides an unparalleled toolkit to manage your overall health and prevent the acute crises that lead to hospitalisation.
Think of it this way: the policy doesn't manage the chronic fire, but it gives you the industry's best fire extinguisher to stop it from burning down the house. It's about preventing new, related (or unrelated) acute conditions from developing and stopping a chronic condition from escalating into an acute emergency.
Your PMI Toolkit for Proactive Health Management
Modern PMI is less a simple insurance policy and more a comprehensive health and wellbeing partnership. It provides swift access to services that can detect issues early, intervene rapidly, and support healthier lifestyles—the three pillars of preventing avoidable hospital admissions.
| Feature | NHS Pathway (Potential Experience) | PMI Pathway (Typical Experience) | Impact on Preventing Avoidable Admissions |
|---|---|---|---|
| GP Access | Days or weeks for a routine appointment. | Same-day or 24/7 virtual GP access. | Catches issues early before they escalate. |
| Specialist Referral | Weeks or months wait for a consultation. | Referral and appointment within days. | Rapid diagnosis and treatment plan prevents deterioration. |
| Diagnostic Scans | Weeks or months wait for MRI/CT scans. | Scans often completed within a week. | Early and precise diagnosis of potential problems. |
| Mental Health | Long waits for therapy (IAPT services). | Rapid access to a network of therapists. | Addresses stress/anxiety that can worsen physical conditions. |
| Wellbeing Support | Limited access to nutritionists/physios. | Often included; discounts on gyms, health apps. | Empowers proactive lifestyle changes to manage risk. |
Advanced Diagnostics: Seeing the Problem Before It Starts
Imagine you're experiencing intermittent chest pain. On the NHS, you might face a significant wait for an ECG and a subsequent referral to a cardiologist, followed by another wait for advanced imaging like a CT angiogram.
With a comprehensive PMI plan, a virtual GP could refer you to a private cardiologist within a week. That specialist could then approve a state-of-the-art scan, which you might have in the next few days. This process could uncover early-stage coronary artery disease, allowing for immediate intervention with medication and lifestyle changes, thereby preventing a future heart attack and a life-changing hospital admission.
Rapid Access to Specialists: Intervention When It Counts
Let's return to the person with Type 2 diabetes. Their blood sugar levels are becoming erratic. Getting a timely NHS appointment with an endocrinologist to fine-tune their medication could take months. In that time, they are at high risk of a hyperglycaemic event requiring hospitalisation.
With PMI, they can see a private endocrinologist quickly. The specialist can adjust their treatment plan, provide education on new monitoring technology, and connect them with a nutritionist—all within a matter of weeks. This rapid, coordinated care can stabilise their condition and dramatically reduce the risk of an avoidable, emergency admission.
A Commitment Beyond the Policy: The WeCovr Approach
At WeCovr, we believe that empowering our clients to live healthier lives is fundamental. We see insurance as one part of a wider health strategy. This is why, in addition to our core service of helping you compare plans and find the perfect cover, we go a step further.
As a WeCovr customer, you receive complimentary access to CalorieHero, our exclusive, AI-powered calorie and nutrition tracking app. Managing weight and nutrition is one of the single most effective ways to reduce the risk of numerous chronic conditions, from heart disease to Type 2 diabetes. By providing this tool, we are actively investing in your long-term health, helping you build the foundations of wellbeing that prevent illness from taking hold in the first place.
Navigating the Market: Finding the Right PMI for Your Family's Future
Choosing a PMI policy is a significant decision. The market is complex, with different providers emphasising different aspects of care. Understanding the key variables is essential.
Key Considerations When Choosing a Policy
- Level of Cover: Policies are typically tiered. Basic plans might only cover in-patient treatment, while comprehensive plans include out-patient diagnostics, therapies, and extensive mental health support.
- Underwriting Type:
- Moratorium: Simpler to set up. Insurers won't cover any condition you've had in the last 5 years until you go 2 full years without symptoms or treatment for it.
- Full Medical Underwriting (FMU): You disclose your full medical history. The insurer then explicitly states what is and isn't covered from the outset.
- Hospital List: Insurers have different lists of approved hospitals. Ensure the hospitals convenient for you are included.
- Excess: This is the amount you agree to pay towards a claim. A higher excess will lower your monthly premium.
The Value of an Expert Broker
Navigating this landscape alone can be daunting. The policy documents are complex, and the long-term implications of choosing the wrong plan can be significant. This is where an independent, expert broker like WeCovr becomes invaluable.
Our role is to:
- Understand Your Needs: We take the time to learn about your family's health concerns, your budget, and your priorities.
- Scan the Entire Market: We compare plans from all the UK's leading insurers, including Bupa, AXA Health, Aviva, and Vitality, ensuring you see the full range of options.
- Demystify the Jargon: We explain the differences between policies in plain English, so you can make a truly informed decision.
- Advocate for You: We help you find a policy that doesn't just offer treatment, but provides the proactive, preventative tools you need to protect your family's future.
Comparing Leading UK Insurer Approaches to Preventative Health
Different insurers have unique strengths when it comes to wellbeing.
| Insurer | Key Preventative/Wellbeing Focus | Example Benefit |
|---|---|---|
| Bupa | Comprehensive health assessments and mental health support. | Access to the Bupa Live Well programme and extensive mental health cover. |
| AXA Health | Strong focus on digital GP and fast-track specialist access. | The "Doctor at Hand" service providing 24/7 virtual GP consultations. |
| Aviva | Integrated approach with a focus on expert diagnostics. | The "Aviva Digital GP" app and access to their Expert Select hospital network. |
| Vitality | Gamified wellness programme rewarding healthy behaviour. | Active Rewards programme with points for exercise, offering discounts and perks. |
Note: Specific benefits and programmes are subject to change and policy terms.
An expert broker can help you weigh these different philosophies against your personal preferences to find the perfect fit.
Conclusion: Taking Control of Your Health Trajectory
The 2025 data is not a forecast of doom but a call to action. It reveals the profound and growing gap between reactive and proactive healthcare. Relying solely on a system that is, by necessity, focused on treating acute illness is a gamble that a third of families are currently losing.
An avoidable hospital admission is a life-altering event with a devastating personal and financial cost. Preventing it requires a fundamental shift in mindset—from waiting for sickness to actively pursuing wellness.
While it is crucial to remember that Private Medical Insurance does not cover pre-existing or chronic conditions, it is unequivocally one of the most powerful tools available for this proactive mission. The ability to bypass diagnostic queues, get rapid access to the UK's top specialists, and utilise a suite of integrated wellbeing and mental health tools can be the difference between managing a condition effectively and facing an emergency crisis.
Protecting your family’s future is about more than just financial planning; it’s about health planning. By understanding the risks and exploring the tools at your disposal, you can build a robust shield against avoidable illness, preserving not just your finances, but the health, independence, and quality of life you and your loved ones deserve.
Sources
- NHS England: Waiting times and referral-to-treatment statistics.
- Office for National Statistics (ONS): Health, mortality, and workforce data.
- NICE: Clinical guidance and technology appraisals.
- Care Quality Commission (CQC): Provider quality and inspection reports.
- UK Health Security Agency (UKHSA): Public health surveillance reports.
- Association of British Insurers (ABI): Health and protection market publications.