TL;DR
The United Kingdom is facing a silent but escalating health crisis. It’s not a new virus or a sudden pandemic, but a slow-burning "time bomb" ticking away within our cherished National Health Service. New analysis based on 2025 health trends reveals a shocking statistic: as many as one in three new chronic illness diagnoses could have been prevented or their severity dramatically reduced with earlier intervention.
Key takeaways
- Core Cover (Basic): This is the foundation of every policy. It covers the most expensive aspects of healthcare: in-patient and day-patient treatment. This means if you need to be admitted to a hospital for surgery or a procedure, the costs for surgeons, anaesthetists, and the hospital room are covered. Comprehensive cancer cover is often included as standard or as a key option at this level.
- Mid-Range Cover: This level builds on the core by adding out-patient benefits. This is a crucial addition, as it covers the costs of the diagnostic journey: specialist consultations and scans (MRI, CT, etc.) that happen before any hospital admission. For many, this is the most valuable part of the policy.
- Comprehensive Cover: This is the top tier. It includes everything from the lower levels and adds more extensive benefits, such as therapies (physiotherapy, osteopathy, chiropody), mental health support (psychiatry and therapy sessions), and sometimes alternative therapies.
- Moratorium Underwriting (Most Common): You don't declare your medical history upfront. Instead, the policy automatically excludes any condition you've had symptoms, treatment, or advice for in the 5 years before your policy starts. This exclusion is usually lifted if you go 2 full years on the policy without any further symptoms, treatment, or advice for that condition. It's simple and quick.
- Full Medical Underwriting (FMU): You complete a detailed health questionnaire. The insurer assesses your history and lists specific, permanent exclusions from the outset. It takes longer but provides absolute clarity on what is and isn't covered from day one.
UK Health Time Bomb 1 in 3 Avoidable Chronic Illnesses
The United Kingdom is facing a silent but escalating health crisis. It’s not a new virus or a sudden pandemic, but a slow-burning "time bomb" ticking away within our cherished National Health Service. New analysis based on 2025 health trends reveals a shocking statistic: as many as one in three new chronic illness diagnoses could have been prevented or their severity dramatically reduced with earlier intervention.
For millions, the journey from a simple, treatable symptom to a lifelong, debilitating condition is being paved by record-breaking NHS waiting lists. A nagging pain, a worrying lump, or a persistent low mood, once addressed promptly, now risks festering for months, even years, before a diagnosis is made. By then, an acute, solvable problem may have morphed into a chronic, uninsurable illness that permanently alters one's quality of life.
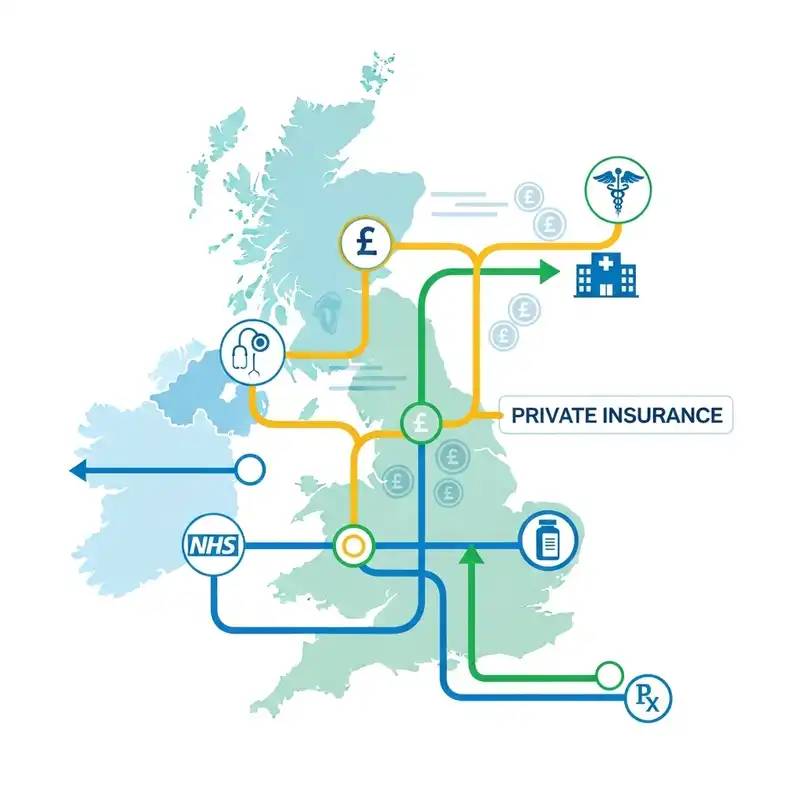
This is where the paradigm of healthcare in the UK is shifting. While the NHS remains the bedrock of emergency care, a growing number of Britons are turning to Private Medical Insurance (PMI) not as a luxury, but as a vital tool for proactive health management.
This definitive guide will unpack the latest 2025 data, explore the critical link between NHS delays and the rise of preventable chronic disease, and demonstrate how PMI can empower you to defuse your personal health time bomb through rapid diagnostics and early treatment.
The UK's Health Time Bomb: The 2025 Data Unpacked
The term "time bomb" is not hyperbole. It reflects a dangerous cascade effect where delays in healthcare directly lead to poorer long-term health outcomes. A landmark 2025 report by the Health Foundation, titled "The Ticking Clock," synthesises data from the Office for National Statistics (ONS) and NHS Digital to paint a sobering picture.
The report’s headline finding is that an estimated 34% of new chronic condition diagnoses in the past year—including Type 2 diabetes, severe osteoarthritis, certain cardiovascular diseases, and chronic mental health disorders—could have been avoided or significantly mitigated if the patient had received a diagnosis and treatment within clinically recommended timeframes.
What's driving this crisis?
- Diagnostic Delays: The average wait for a routine MRI scan on the NHS has stretched to 14 weeks in some regions, up from 6 weeks pre-pandemic. For conditions like persistent joint pain, this delay can be the difference between successful physiotherapy and the need for a joint replacement.
- Referral to Treatment (RTT) Times: The 18-week RTT pathway, a cornerstone of NHS targets, is now an ambition rather than a reality for millions. The overall waiting list in England alone now sits at a staggering 7.8 million people, with many waiting over a year for treatment.
- GP Access: While GPs are working harder than ever, securing a timely appointment to even begin the diagnostic journey has become a significant hurdle, creating a bottleneck at the very start of the care pathway.
The Cascade Effect: How Acute Symptoms Become Chronic Nightmares
The danger lies in how easily treatable, acute issues can become permanent, chronic conditions when left unattended. This is the crux of the problem.
Consider the following common scenarios, which illustrate the stark difference between the NHS and PMI pathways in 2025.
| Acute Symptom | Typical NHS Pathway & 2025 Wait Time | Potential Chronic Outcome | Typical PMI Pathway & Wait Time | Mitigated Outcome |
|---|---|---|---|---|
| Persistent Knee Pain | GP wait (2-3 weeks), Physio referral wait (8-12 weeks), MRI wait if needed (10-14 weeks) | Cartilage wears away, leading to severe, chronic osteoarthritis and eventual joint replacement. | Virtual GP (same day), Private MRI (within 1 week), Specialist consult (within 2 weeks) | Early physio, injections or minor arthroscopic surgery preserves the joint. |
| Changes in Bowel Habits | GP wait (2-3 weeks), Urgent 2-week-wait cancer referral (often met, but diagnostic colonoscopy wait can be 6-8 weeks) | A treatable polyp can become cancerous; early-stage bowel cancer can advance. | Fast-track consultant referral (days), Private colonoscopy (within 1-2 weeks) | Polpys removed before they turn cancerous; early detection dramatically improves prognosis. |
| Low Mood & Anxiety | GP wait (2-3 weeks), Referral to IAPT/Talking Therapies (12-18 week wait for first session) | Symptoms worsen, leading to severe depression/anxiety, inability to work, relationship breakdown. | Virtual GP (same day), Direct access to private therapy/psychiatry (within 1-2 weeks) | Early intervention with therapy/medication prevents escalation, enabling a faster return to full function. |
| Heavy/Painful Periods | GP wait (2-3 weeks), Gynaecology referral wait (20-30 weeks), Ultrasound wait (8-10 weeks) | Untreated conditions like endometriosis or fibroids worsen, causing chronic pain and fertility issues. | GP referral to private gynaecologist (within 1 week), Private ultrasound (days) | Early diagnosis and treatment (e.g., laparoscopy, medication) manages symptoms and preserves fertility. |
This table clearly shows the "time bomb" in action. The window of opportunity to treat an issue while it is still acute and reversible is closing for many on standard pathways.
The NHS in 2025: A System Under Unprecedented Strain
To understand why PMI is becoming so essential, we must first appreciate the scale of the challenge facing the NHS. It remains one of the world's finest healthcare systems for emergency and critical care. If you have a heart attack or are in a serious accident, the NHS is magnificent. The current crisis, however, is centred on elective care, diagnostics, and the management of non-life-threatening (but life-altering) conditions.
Key Pressure Points in 2025:
This "hidden" waiting list doesn't even account for those who haven't yet been referred by their GP.
- The Cancer Backlog: While urgent cancer referrals are prioritised, the strain on diagnostic services (radiology, endoscopy) means there are still significant delays in the 62-day pathway from referral to treatment. Cancer Research UK has warned that every month of delay can impact survival rates.
- Workforce Shortages: The system is grappling with significant staff shortages across key specialities, from radiologists to nurses to anaesthetists, further limiting its capacity to clear the backlog.
- The Human Cost: Beyond the statistics, there is a profound human cost. People are living in pain, unable to work, and suffering from the immense anxiety of not knowing what is wrong with them. A 2025 survey by Mind revealed that 65% of people on a long-term physical health waiting list reported a significant decline in their mental health.
Real-Life Example: David's Story
David, a 52-year-old self-employed plumber, began experiencing severe shoulder pain in late 2023. His GP suspected a rotator cuff tear and referred him for an ultrasound. He was told the NHS wait would be four months. Unable to lift his arm properly, he couldn't work. The loss of income was devastating, and the constant pain made sleep impossible.
Frustrated, David used his savings to pay for a private consultation (£250) and an ultrasound (£350), which he got within a week. The scan confirmed a significant tear requiring surgery. The NHS surgical waiting list was over 18 months. Faced with financial ruin, he took out a loan to pay for private surgery (£6,000).
David's story is increasingly common. He was fortunate to have savings and access to credit. For many, the only option is to wait, while their health, finances, and wellbeing deteriorate. This is the gap that Private Medical Insurance is designed to fill.
Private Medical Insurance (PMI): Your Proactive Health Partner
It is essential to view Private Medical Insurance not as a rejection of the NHS, but as a complementary partner that works alongside it. You will still use the NHS for accidents and emergencies, for managing long-term chronic conditions, and for GP services if you wish.
PMI's primary role is to bypass the queues for non-emergency, acute conditions. It provides a parallel track that offers speed, choice, and control when you need it most.
How PMI Defuses the Time Bomb:
- Rapid Diagnostics: This is arguably the most significant benefit in today's climate. A PMI policy can give you access to an MRI, CT scan, or ultrasound within days of a GP referral, providing a swift and accurate diagnosis.
- Prompt Specialist Access: Instead of waiting months to see a consultant, you can typically see a specialist of your choice within a week or two, allowing a treatment plan to be formulated immediately.
- Fast-Track Treatment: Once a diagnosis is made, PMI provides access to treatment—be it surgery, therapy, or another intervention—at a private hospital at a time that suits you, often within a few weeks.
- Choice and Comfort: PMI offers the ability to choose your surgeon or specialist and recover in the comfort of a private room, reducing stress and aiding recovery.
NHS vs. PMI: A 2025 Timeline Comparison
The difference in timescales is the core value proposition of private cover.
| Healthcare Stage | Average NHS Wait Time (2025 data) | Average PMI Wait Time |
|---|---|---|
| Initial GP Referral to Specialist | 18 - 22 weeks | 1 - 2 weeks |
| Specialist to Diagnostic Scan (MRI/CT) | 10 - 14 weeks | 3 - 7 days |
| Diagnosis to Treatment (e.g., Surgery) | 25 - 52+ weeks | 2 - 4 weeks |
| Access to Mental Health Therapy | 12 - 18 weeks | 1 - 2 weeks |
| Access to Physiotherapy | 8 - 12 weeks | 3 - 7 days |
The conclusion is inescapable: PMI grants you access to medical intervention in a fraction of the time, tackling health problems while they are small, manageable, and acute.
The Crucial Distinction: Acute vs. Chronic Conditions
This is the single most important concept to understand about UK Private Medical Insurance. Misunderstanding this point can lead to disappointment and frustration.
PMI is designed to cover acute conditions that arise after you take out your policy.
- An Acute Condition: Is a disease, illness, or injury that is short-term in nature. It is expected that you will respond to treatment and make a full recovery, or be returned to your previous state of health. Examples include cataracts, hernias, joint sprains, gallstones, and diagnosing new symptoms.
- A Chronic Condition: Is a condition that is long-lasting and requires ongoing or long-term monitoring and management. It cannot be 'cured' in the traditional sense, only managed. Examples include diabetes, asthma, Crohn's disease, arthritis, and high blood pressure.
The Golden Rule of UK Health Insurance
Standard Private Medical Insurance policies DO NOT cover pre-existing conditions or the ongoing management of chronic conditions.
If you have diabetes before you take out a policy, the PMI will not pay for your insulin or regular check-ups. If you are diagnosed with a chronic condition like rheumatoid arthritis while you have a policy, the insurer will typically pay for the initial diagnosis and stabilisation treatment. However, the long-term, day-to-day management of that condition will then revert to the NHS.
The reason for this is simple. Insurance works on the principle of covering unforeseen events. A pre-existing or chronic condition is a known certainty, not an unknown risk, making it uninsurable in the standard market.
This is precisely why PMI is so critical as a preventative tool. Its value lies in getting you treated for an acute issue (like a torn ligament) so quickly that you avoid it developing into a chronic one (like permanent joint instability and arthritis). It keeps you in the "insurable" category by tackling problems head-on.
What Does a Typical PMI Policy Cover?
Policies are not one-size-fits-all. They are typically structured in tiers, allowing you to balance the level of cover with your budget.
- Core Cover (Basic): This is the foundation of every policy. It covers the most expensive aspects of healthcare: in-patient and day-patient treatment. This means if you need to be admitted to a hospital for surgery or a procedure, the costs for surgeons, anaesthetists, and the hospital room are covered. Comprehensive cancer cover is often included as standard or as a key option at this level.
- Mid-Range Cover: This level builds on the core by adding out-patient benefits. This is a crucial addition, as it covers the costs of the diagnostic journey: specialist consultations and scans (MRI, CT, etc.) that happen before any hospital admission. For many, this is the most valuable part of the policy.
- Comprehensive Cover: This is the top tier. It includes everything from the lower levels and adds more extensive benefits, such as therapies (physiotherapy, osteopathy, chiropody), mental health support (psychiatry and therapy sessions), and sometimes alternative therapies.
Levels of PMI Cover Explained
| Feature | Basic Cover | Mid-Range Cover | Comprehensive Cover |
|---|---|---|---|
| In-Patient & Day-Patient Care | ✔️ Yes | ✔️ Yes | ✔️ Yes |
| Comprehensive Cancer Cover | ✔️ Often Standard | ✔️ Yes | ✔️ Yes |
| Out-Patient Consultations & Scans | ❌ No | ✔️ Yes (often up to a limit) | ✔️ Yes (often in full) |
| Therapies (e.g., Physio) | ❌ No | ❌ No | ✔️ Yes |
| Mental Health Cover | ❌ No | ➕ Optional Add-on | ✔️ Often Included |
| Virtual GP Services | ✔️ Often Standard | ✔️ Yes | ✔️ Yes |
You can further tailor your policy with options like dental and optical cover, travel insurance, and by choosing a specific list of hospitals you have access to.
Unlocking Value: Beyond the Core Policy
In 2025, a good PMI policy is more than just a passport to fast treatment. Insurers are now focused on keeping you healthy, not just treating you when you're ill. This has led to an explosion of value-added benefits that can enhance your daily wellbeing.
- 24/7 Virtual GP Services: Skip the 8am scramble for a GP appointment. Most policies now include an app-based service that gives you and your family access to a GP by video call, 24/7, often with the ability to get prescriptions, sick notes, and referrals.
- Mental Health Support: Beyond full-cover therapy, many policies offer access to confidential helplines and a set number of counselling sessions without needing a GP referral, providing immediate support for stress, anxiety, and other concerns.
- Wellness and Rewards Programmes: Insurers like Vitality have pioneered rewarding members for healthy living, offering discounts on gym memberships, fitness trackers, and healthy food in return for being active.
Many modern policies, like those we help you compare at WeCovr, come bundled with these valuable digital health tools, transforming your insurance from a reactive safety net into a proactive wellness partner.
At WeCovr, we believe in going the extra mile for our clients' health. That's why, in addition to finding you the perfect policy, we provide complimentary access to our exclusive AI-powered calorie and nutrition tracker, CalorieHero. It's our way of helping you manage your health proactively, every single day, empowering you with the knowledge to make healthier choices that can prevent illness in the first place.
The Financial Equation: Is PMI Worth the Investment?
The cost of a PMI policy can vary significantly based on a few key factors:
- Age: Premiums increase as you get older.
- Location: Costs are typically higher in Central London and major cities where hospital fees are more expensive.
- Level of Cover: A comprehensive policy will cost more than a basic one.
- Policy Options: Adding extras or choosing a more extensive hospital list increases the price.
- Excess (illustrative): This is a sum you agree to pay towards any claim, similar to car insurance. A higher excess (£500 or £1,000) can significantly reduce your monthly premium.
- Lifestyle: Smokers will pay more than non-smokers.
Estimated Monthly PMI Premiums (2025)
This table provides a rough guide for a non-smoker outside London with a £250 excess. (illustrative estimate)
| Age | Basic Core Cover (In-patient only) | Comprehensive Cover (Out-patient & Therapies) |
|---|---|---|
| 30s | £30 - £45 | £60 - £85 |
| 40s | £45 - £60 | £80 - £110 |
| 50s | £65 - £90 | £120 - £170 |
| 60s | £100 - £150 | £180 - £250+ |
When considering the cost, it's crucial to weigh it against the alternative. A single private knee replacement can cost over £15,000. A private MRI scan is £400-£800. More importantly, what is the cost of lost earnings while you wait for treatment? What is the cost to your quality of life of living in pain or with constant anxiety? For many, the monthly premium is a small price to pay for peace of mind and the assurance of rapid medical care. (illustrative estimate)
How to Choose the Right PMI Policy for You
The UK health insurance market is complex, with dozens of policies from insurers like Aviva, AXA Health, Bupa, The Exeter, and Vitality. Here’s a simple process to find the right cover.
Step 1: Assess Your Needs and Budget What's your priority? Is it fast access to diagnostics? Comprehensive cancer cover? Mental health support? Or simply a backstop for major surgical procedures? Decide on a monthly budget you are comfortable with.
Step 2: Understand Underwriting This determines how the insurer treats your pre-existing medical conditions. You have two main choices:
- Moratorium Underwriting (Most Common): You don't declare your medical history upfront. Instead, the policy automatically excludes any condition you've had symptoms, treatment, or advice for in the 5 years before your policy starts. This exclusion is usually lifted if you go 2 full years on the policy without any further symptoms, treatment, or advice for that condition. It's simple and quick.
- Full Medical Underwriting (FMU): You complete a detailed health questionnaire. The insurer assesses your history and lists specific, permanent exclusions from the outset. It takes longer but provides absolute clarity on what is and isn't covered from day one.
Step 3: Compare Key Policy Details Don't just look at the headline price. Compare the out-patient limits, the type of cancer cover (does it cover experimental drugs?), the hospital list, and the value-added benefits.
Step 4: Use an Independent, Expert Broker Navigating this complex market can be daunting. This is where an independent, expert broker like us at WeCovr becomes invaluable. An expert broker doesn't just sell you a policy; they provide a crucial advice service. We compare plans from across the entire market, explain the jargon, and find a policy that aligns perfectly with your needs and budget, ensuring there are no nasty surprises down the line. We do the hard work for you, at no extra cost.
Conclusion: Taking Control of Your Health in an Uncertain World
The evidence from 2025 is clear: the landscape of UK healthcare is changing. While the NHS continues to provide world-class emergency care, the delays in the system are creating a preventable public health crisis, turning treatable acute conditions into life-limiting chronic illnesses.
Waiting is no longer a passive activity; it is an active risk to your long-term health.
Private Medical Insurance has evolved from a 'nice-to-have' perk into an essential tool for anyone who wants to take a proactive stance on their wellbeing. It offers the speed, choice, and control needed to get diagnosed early and treated quickly, effectively intervening before a minor issue becomes a major problem.
By understanding that PMI is there for acute conditions—and that its greatest power is in preventing them from becoming chronic—you can use it as a strategic investment. It is an investment in your ability to work, to enjoy your life free from pain and worry, and to safeguard your most precious asset: your future health. In an increasingly uncertain world, taking control of what you can is not just smart; it's essential.
Sources
- NHS England: Waiting times and referral-to-treatment statistics.
- Office for National Statistics (ONS): Health, mortality, and workforce data.
- NICE: Clinical guidance and technology appraisals.
- Care Quality Commission (CQC): Provider quality and inspection reports.
- UK Health Security Agency (UKHSA): Public health surveillance reports.
- Association of British Insurers (ABI): Health and protection market publications.