TL;DR
The numbers are in, and they paint a sobering picture of the UK’s health. Fresh data for 2025 reveals a startling statistic: over 60% of adults in the United Kingdom are now classified as either overweight or obese. This isn't just a headline; it's a ticking disease time bomb with profound implications for millions of individuals and the National Health Service (NHS) that supports them.
Key takeaways
- Record Waiting Lists: The overall waiting list for elective NHS treatment in England continues to hover around the 7.5 million mark.
- Diagnostic Delays: Millions are waiting for crucial diagnostic tests like MRIs, CT scans, and endoscopies—the very tools needed to catch conditions early.
- Long Waits for Treatment: The wait for routine but life-changing operations like knee and hip replacements—procedures frequently necessitated by obesity—can stretch for well over a year in many parts of the country.
- Pre-diabetes: If caught early through blood tests, it can often be reversed with lifestyle changes. If left undiagnosed due to long waits, it can progress to full-blown Type 2 diabetes, a lifelong chronic condition.
- Knee Pain: Early intervention with physiotherapy and specialist advice can preserve a joint. A year-long wait can result in irreversible cartilage damage, making major surgery the only option.
UK Obesity Disease Time Bomb
The numbers are in, and they paint a sobering picture of the UK’s health. Fresh data for 2025 reveals a startling statistic: over 60% of adults in the United Kingdom are now classified as either overweight or obese. This isn't just a headline; it's a ticking disease time bomb with profound implications for millions of individuals and the National Health Service (NHS) that supports them.
For decades, we’ve discussed rising obesity rates. Now, we are living with the consequences. This isn't a future problem; it's a present-day crisis manifesting as soaring rates of Type 2 diabetes, heart disease, certain cancers, and debilitating joint conditions. These aren't abstract health issues; they are personal health crises that diminish quality of life, shorten lifespans, and place an unprecedented strain on our public healthcare system.
The sheer scale of the problem means the traditional, reactive approach to healthcare—waiting for symptoms to become severe before seeking help—is no longer a viable strategy. NHS waiting lists are at record highs, and for conditions where early intervention is critical, these delays can be devastating.
But what if there was another way? A proactive pathway that empowers you to get ahead of potential health problems, provides the tools to manage your well-being, and guarantees swift access to expert medical care when you need it most?
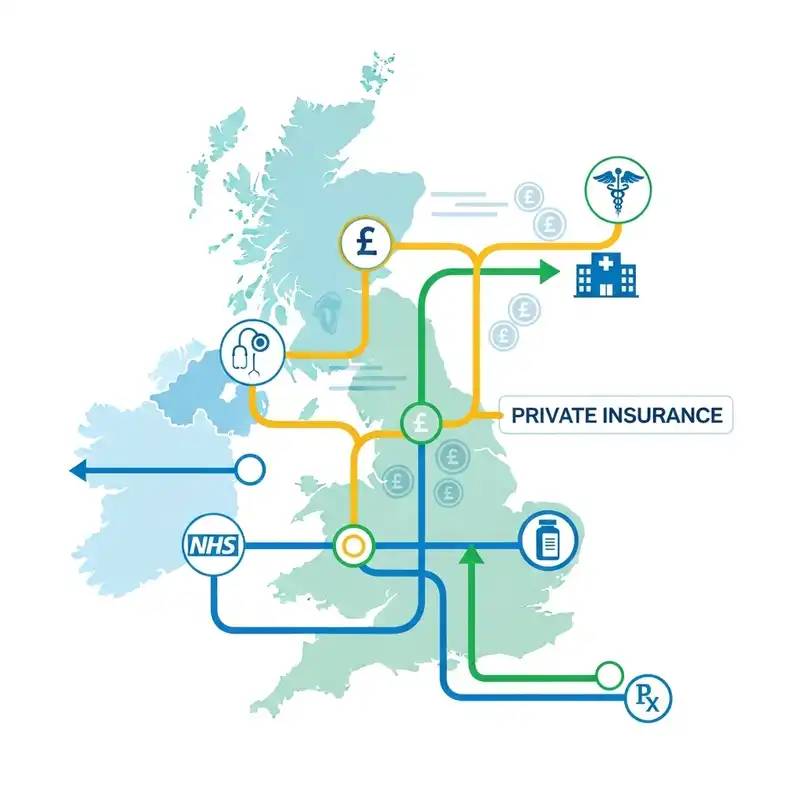
This is where Private Medical Insurance (PMI) enters the conversation. Far from being a simple 'queue-jumping' service, modern health insurance has evolved into a powerful tool for preventative health. It offers a structured, supportive, and rapid route to diagnostics, specialist consultations, and treatments that can help you prevent and, in some cases, reverse the trajectory of your personal health crisis.
In this definitive guide, we will unpack the stark reality of the UK's obesity epidemic, explore the cascade of related health conditions, and provide a clear, in-depth look at how a private health insurance policy can serve as your most valuable ally in taking control of your health narrative.
The Stark Reality: Unpacking the UK's Obesity Statistics
To truly grasp the challenge, we must first understand the numbers. The latest figures are not just statistics on a page; they represent real people, families, and communities across the nation.
- 64.3% of Adults: Approximately two-thirds of the UK adult population are either overweight (a Body Mass Index [BMI] of 25 to 29.9) or obese (a BMI of 30 or above).
- Obesity Prevalence: Of this figure, an alarming 28.7% of adults are classified as obese, with 4.8% being morbidly obese (BMI of 40 or over).
- Regional Disparities: The problem is not uniform. The North East of England continues to have the highest rates of obesity, with over 34% of its adult population being obese, compared to London, which has the lowest rate at around 24%.
- Age and Obesity: The likelihood of being overweight or obese increases significantly with age. While around 45% of 18-24 year-olds are overweight, this figure climbs to over 75% in the 55-64 age bracket.
This escalating trend puts the UK among the most overweight nations in Western Europe, a league table we should not aspire to top.
UK Adult Obesity & Overweight Statistics (2025 Estimates)
| Metric | Statistic | Source |
|---|---|---|
| Overweight or Obese | 64.3% of Adults | NHS Digital |
| Obese | 28.7% of Adults | NHS Digital |
| Morbidly Obese | 4.8% of Adults | The Lancet |
| Highest Regional Rate | 34.1% (North East) | Public Health England |
| Lowest Regional Rate | 24.2% (London) | Public Health England |
| Impact on NHS Costs | Est. £9.8 billion annually (direct & indirect) | ONS |
The financial cost is staggering, but the human cost is immeasurable. Behind each percentage point are individuals facing a significantly higher risk of developing a host of serious, life-altering medical conditions.
More Than Just Weight: The Cascade of Obesity-Related Health Conditions
The term "obesity" is often misunderstood as a simple issue of weight or appearance. In medical terms, it is a complex, chronic disease that acts as a primary catalyst for a wide range of other serious health problems. Excess body fat, particularly visceral fat around the organs, is metabolically active. It releases inflammatory substances and hormones that disrupt the body's normal functions, creating a domino effect of ill health.
This isn't a potential risk; it's a proven medical link. Let's examine the most common and dangerous co-morbidities.
1. Type 2 Diabetes: This is perhaps the most well-known complication. Obesity is the single biggest risk factor for developing Type 2 diabetes. Excess fat can cause insulin resistance, a state where the body's cells don't respond effectively to insulin. This forces the pancreas to work harder until it eventually can't keep up, leading to high blood sugar levels that damage nerves, blood vessels, kidneys, and eyes.
2. Cardiovascular Disease: The link is direct and deadly. Obesity contributes to:
- High Blood Pressure (Hypertension): The heart has to pump harder to supply blood to a larger body mass.
- High Cholesterol: Obesity is associated with higher levels of "bad" LDL cholesterol and lower levels of "good" HDL cholesterol, leading to the build-up of fatty plaques in the arteries (atherosclerosis).
- Heart Attacks & Strokes: Atherosclerosis narrows the arteries, increasing the risk of blood clots that can cause a heart attack or stroke.
3. Cancer: The evidence is now undeniable. Cancer Research UK estimates that obesity is the second biggest preventable cause of cancer after smoking. It is linked to at least 13 different types of cancer, including:
- Bowel cancer
- Pancreatic cancer
- Kidney cancer
- Liver cancer
- Oesophageal cancer
- Post-menopausal breast cancer
4. Musculoskeletal Problems: Carrying excess weight places immense strain on the body's framework, particularly the joints. This leads to:
- Osteoarthritis: The protective cartilage in joints like the knees, hips, and lower back wears down faster, causing chronic pain, stiffness, and reduced mobility. This often necessitates joint replacement surgery.
- Gout: A painful form of inflammatory arthritis linked to high levels of uric acid, which is more common in overweight individuals.
5. Respiratory & Sleep Issues:
- Sleep Apnoea: Excess fatty tissue in the neck can obstruct the airway during sleep, causing breathing to repeatedly stop and start. This leads to poor sleep quality, daytime fatigue, and increased strain on the heart.
- Asthma: Obesity can worsen asthma symptoms and make attacks more severe.
6. Mental Health Conditions: The connection is a two-way street. People with obesity are more likely to suffer from depression, anxiety, and low self-esteem due to social stigma and physical limitations. Conversely, mental health issues can contribute to weight gain through comfort eating or lack of motivation.
The Link Between Obesity and Chronic Disease
| Condition | How Obesity Contributes | Impact on Quality of Life |
|---|---|---|
| Type 2 Diabetes | Causes insulin resistance | Daily monitoring, medication, risk of complications |
| Heart Disease & Stroke | Increases blood pressure and "bad" cholesterol | Medication, risk of sudden life-threatening events |
| Certain Cancers | Promotes inflammation and abnormal cell growth | Invasive treatments, significant impact on life expectancy |
| Osteoarthritis | Places mechanical stress on joints, wearing down cartilage | Chronic pain, loss of mobility, need for major surgery |
| Sleep Apnoea | Fatty tissue obstructs the airway during sleep | Severe fatigue, poor concentration, long-term heart strain |
| Depression & Anxiety | Social stigma, physical discomfort, and hormonal changes | Reduced emotional well-being, affects daily functioning |
This cascade of illness not only impacts individuals but also creates a tidal wave of demand that crashes against the services of our beloved NHS.
The NHS Under Strain: Why Waiting Isn't a Viable Strategy
The National Health Service is one of the UK's greatest achievements, providing care to all, free at the point of use. However, it was designed in an era before the current obesity-driven chronic disease epidemic. Today, it is operating under unprecedented pressure.
As of mid-2025, the reality is stark:
- Record Waiting Lists: The overall waiting list for elective NHS treatment in England continues to hover around the 7.5 million mark.
- Diagnostic Delays: Millions are waiting for crucial diagnostic tests like MRIs, CT scans, and endoscopies—the very tools needed to catch conditions early.
- Long Waits for Treatment: The wait for routine but life-changing operations like knee and hip replacements—procedures frequently necessitated by obesity—can stretch for well over a year in many parts of the country.
For the health conditions we've just discussed, time is the most critical factor.
- Pre-diabetes: If caught early through blood tests, it can often be reversed with lifestyle changes. If left undiagnosed due to long waits, it can progress to full-blown Type 2 diabetes, a lifelong chronic condition.
- Knee Pain: Early intervention with physiotherapy and specialist advice can preserve a joint. A year-long wait can result in irreversible cartilage damage, making major surgery the only option.
- Suspicious Symptoms: A delay in seeing a specialist or getting a scan for symptoms that could indicate cancer can be the difference between a treatable diagnosis and a terminal one.
Relying solely on an overstretched system for proactive and timely care is, for many, a high-stakes gamble. This is not a criticism of the hardworking NHS staff, but a pragmatic assessment of the system's capacity. It highlights the urgent need for a parallel, proactive approach that puts you in the driver's seat of your health.
The Proactive Pathway: How Private Medical Insurance Empowers Your Health Journey
This is where the narrative shifts from problem to solution. Private Medical Insurance (PMI) is a powerful tool that enables a proactive, rather than reactive, approach to your health. It provides the resources, access, and support to manage your well-being and tackle health issues head-on, before they escalate.
However, before we explore the benefits, we must address a critical and non-negotiable rule of UK health insurance.
⚠️ The Golden Rule: PMI Does Not Cover Pre-Existing or Chronic Conditions
Let's be unequivocally clear: Standard Private Medical Insurance is designed to cover acute conditions that arise after your policy begins.
- An acute condition is a disease, illness, or injury that is likely to respond quickly to treatment and lead to a full recovery (e.g., a cataract, a hernia, a joint injury).
- A chronic condition is a disease, illness, or injury that has one or more of the following characteristics: it needs long-term monitoring, has no known cure, is likely to recur, or requires ongoing management (e.g., diabetes, hypertension, asthma, osteoarthritis).
- A pre-existing condition is any ailment for which you have experienced symptoms, received medication, or sought advice from a medical professional in the years leading up to your policy start date.
If you are already diagnosed with obesity-related chronic conditions like Type 2 diabetes or established osteoarthritis, a new PMI policy will not cover the management of these specific issues.
So, how can PMI help? It empowers you at a crucial stage: when you are overweight or concerned about your health, but have not yet been diagnosed with a chronic condition. It is a forward-looking tool to manage future, unknown risks and to access services that promote better health now.
Here’s how it works in practice:
1. Prevention and Early Detection
This is PMI's most powerful, yet often overlooked, benefit. Instead of waiting for a GP appointment and then joining a long queue for tests, PMI opens up an express route to answers.
- Swift GP Access: Many policies include access to 24/7 virtual GP services. You can speak to a doctor via phone or video call, often within hours, to discuss concerns like joint pain, fatigue, or worries about your heart health.
- Fast-Track Specialist Referrals: If the GP believes you need to see a specialist—a cardiologist for your heart, an endocrinologist for hormonal issues, or an orthopaedic surgeon for your joints—a private referral can be made immediately. You could be seeing a leading consultant within days, not months.
- Rapid Diagnostics: This is the game-changer. Your policy’s out-patient cover pays for the diagnostic tests needed to get a clear picture of your health. This includes MRIs, CT scans, ultrasounds, blood tests, and heart monitoring (ECGs). Getting these tests done quickly means you can identify problems like high cholesterol, pre-diabetes, or early-stage joint wear and tear at a point where intervention is most effective.
2. Wellness and Lifestyle Support
Modern insurers understand that prevention is better than cure. Most top-tier policies now include a wealth of value-added benefits designed to help you live a healthier life.
- Gym Discounts & Fitness Rewards: Insurers like Vitality famously reward you for being active, offering discounted gym memberships, fitness trackers, and even cinema tickets or coffee for hitting activity goals.
- Nutritionist Consultations: Some plans offer access to registered dietitians who can provide professional, evidence-based advice on weight management and healthy eating—far more effective than generic online advice.
- Mental Health Support: Recognising the link between mind and body, policies increasingly offer access to counselling, therapy, and mental well-being apps to help address the psychological aspects of weight management.
At WeCovr, we believe in going the extra mile for our clients' health. That's why, in addition to finding you the best policy, we provide our customers with complimentary access to CalorieHero, our proprietary AI-powered calorie and nutrition tracking app. It's a practical tool to help you take daily, consistent action towards your health goals, demonstrating our commitment to your long-term well-being.
3. Swift Treatment for New Acute Conditions
If your proactive efforts uncover a new, acute condition, or one develops while you are insured, PMI ensures you get the best possible care without delay.
Imagine your private MRI scan reveals a torn meniscus in your knee, contributing to your pain. Or routine checks uncover gallstones that require surgery. With PMI, you can bypass the NHS waiting list and schedule your treatment at a time and place that suits you.
This includes:
- Choice of Hospital: Access to a network of clean, modern private hospitals with private en-suite rooms.
- Choice of Surgeon: You can research and choose a leading consultant specialist for your procedure.
- Timely Treatment: Your surgery or treatment will be scheduled promptly, minimising time spent in pain and accelerating your recovery.
NHS vs. PMI Pathway: A Hypothetical Scenario
Let's consider a 50-year-old man, David, who is overweight and develops persistent knee pain.
| Stage | NHS Pathway | PMI Pathway |
|---|---|---|
| Initial Consultation | Waits 2-3 weeks for a routine GP appointment. | Uses virtual GP service and speaks to a doctor the same day. |
| Referral | GP refers him to NHS musculoskeletal services. Wait time: 8-12 weeks. | GP provides an open referral to a private orthopaedic consultant. |
| Specialist Appointment | Sees a physiotherapist first. If no improvement, referred to a consultant. Wait: 16-20 weeks. | Sees a consultant of his choice within a week. |
| Diagnostics | Consultant orders an MRI scan. NHS waiting list for MRI: 6-8 weeks. | Consultant orders an MRI. He has the scan at a private clinic two days later. |
| Diagnosis & Plan | Total Wait for Diagnosis: ~9 months. Diagnosis: Torn cartilage & early osteoarthritis. | Total Wait for Diagnosis: ~10 days. Diagnosis: Torn cartilage & early osteoarthritis. |
| Treatment (Surgery) | Placed on the elective surgery waiting list for an arthroscopy. Wait time: 40-52 weeks. | Surgery is scheduled for two weeks' time at a private hospital. |
| Treatment (Therapy) | Referred for NHS physiotherapy. Wait time: 6 weeks. Group sessions. | Physiotherapy is authorised immediately. He begins one-on-one sessions the following week. |
In this scenario, David gets a definitive diagnosis and treatment plan via PMI in less than two weeks. On the NHS, he could still be waiting for his first specialist appointment. This speed is not about luxury; it's about effective medical intervention that prevents a manageable issue from becoming a chronic, debilitating problem.
A Closer Look: What Health Insurance Features Should You Look For?
When considering PMI as a tool for proactive health management, it’s vital to choose a policy with the right features. A "one-size-fits-all" approach doesn't work. Here are the key components to look for, particularly if you are concerned about weight-related health risks.
1. Comprehensive Out-patient Cover: This is arguably the most important feature for proactive care. It covers the costs of specialist consultations and diagnostic tests performed without being admitted to hospital.
- Basic Level (illustrative): May cover just the consultation, or have a low financial limit (e.g., £500).
- Mid-Level (illustrative): A good balance, often with a limit of £1,000 - £1,500. This is usually sufficient for consultations and a round of diagnostics.
- Comprehensive Level: Offers unlimited out-patient cover, giving you complete peace of mind that all necessary tests and consultations will be paid for.
2. Therapies Cover: This covers treatments like physiotherapy, osteopathy, and chiropractic care. For anyone carrying excess weight, musculoskeletal aches and pains are common. Having access to fast, high-quality physiotherapy can manage symptoms, improve mobility, and potentially delay or prevent the need for surgery.
3. Mental Health Cover: Don't underestimate this. The journey to a healthier weight has significant psychological components. Access to professional counselling or therapy can help address emotional eating, build resilience, and support you through lifestyle changes.
4. Wellness and Reward Programmes: Look beyond the core medical cover. Which insurer offers the best proactive benefits? Does the plan include discounts on gym memberships, health screenings, or wearable tech? These "perks" are powerful motivators that encourage the very behaviours that reduce your health risks.
5. Bariatric Surgery Cover (A Note of Caution): Weight loss surgery is a major intervention and is not covered by most standard PMI policies. Some top-tier, comprehensive plans from insurers like Bupa and Aviva may offer cover, but it comes with very strict criteria, such as a high BMI (e.g., over 40), a history of failed weight loss attempts, and a commitment to a full psychological and dietary support programme. It should never be the primary reason for taking out a policy.
Navigating these options can be complex. The terminology is confusing, and the differences between policies are subtle but significant. This is where expert guidance becomes invaluable.
Navigating the Market: The Role of an Expert Broker
You wouldn't navigate a complex legal issue without a solicitor or manage your investments without a financial advisor. Choosing the right health insurance policy is just as important. An expert, independent health insurance broker acts as your advocate and guide.
At WeCovr, our role is to demystify the entire process. We are not tied to any single insurer; our loyalty is to you, our client.
Here’s why using a specialist broker is the smartest approach:
- Whole-of-Market Access: We work with all the major UK insurers, including AXA Health, Bupa, Aviva, Vitality, and The Exeter. We can compare every relevant policy to find the one that truly fits your needs and budget.
- Expert, Tailored Advice: We take the time to understand your personal situation, your health concerns, and what you want to achieve with your policy. We can then recommend the specific features—like high out-patient cover or excellent therapy benefits—that will deliver the most value to you.
- Clarity on the Fine Print: We explain the crucial details of underwriting, exclusions, and policy wording in plain English, so you know exactly what you are and are not covered for. There are no nasty surprises.
- No Extra Cost to You: Our service is free. We are paid a commission by the insurer you choose, which is already built into the premium. You get expert, impartial advice without paying a penny more than if you went direct.
Working with a broker like WeCovr transforms a confusing purchase into a confident, informed decision, ensuring your policy is a robust tool for your future health.
Understanding the Crucial Exclusion: Chronic and Pre-Existing Conditions
We have stated this before, but its importance cannot be overstated. A misunderstanding of this single point is the source of most dissatisfaction with private medical insurance. Let’s break it down with absolute clarity.
PMI is built on a foundation of managing risk for future, unknown, and acute medical conditions.
What is Excluded?
| Type of Condition | Definition | Example | PMI Coverage Status |
|---|---|---|---|
| Pre-Existing | Any medical condition for which you have had symptoms, medication, advice or treatment in the last 5 years. | You saw a GP for knee pain 3 years ago. That knee pain is a pre-existing condition. | Excluded |
| Chronic | A condition that requires long-term management and has no known cure. | Type 2 Diabetes, Hypertension, Crohn's Disease, established Osteoarthritis, Asthma. | Excluded |
This means if you are currently taking medication for high blood pressure, a new PMI policy will not cover your GP check-ups, medication, or any hospital treatment related to your high blood pressure.
How Do Insurers Know? The Two Types of Underwriting
When you apply for a policy, the insurer assesses your risk through a process called underwriting.
1. Moratorium Underwriting (The "Wait and See" Approach):
- This is the most common type. You don't have to declare your full medical history upfront.
- The policy automatically excludes any condition you've had symptoms of or treatment for in the 5 years before the policy started.
- The "2-Year Rule": If you then go for 2 continuous years on the policy without having any symptoms, treatment, or advice for that specific condition, the insurer may reinstate cover for it in the future.
- Best for: People who are generally healthy and want a quicker application process.
2. Full Medical Underwriting (FMU) (The "Full Disclosure" Approach):
- You complete a detailed health questionnaire, declaring your entire medical history.
- The insurer's medical team reviews your application and then tells you upfront exactly what is excluded from your policy, usually for life.
- Best for: People who want absolute certainty from day one about what is and isn't covered, or those who have had a historical medical issue more than 5 years ago that they want to ensure is covered.
Understanding this principle is key: PMI is not a solution for existing health problems. It is a proactive investment in managing your future health risks.
Real-Life Scenarios: How PMI Can Make a Difference
To see the theory in action, let's look at two realistic scenarios.
Case Study 1: Sarah, 45, Office Manager
- The Situation: Sarah has a BMI of 28 (overweight). She has an office job and has started experiencing persistent lower back pain and sciatica, which is affecting her ability to sit, sleep, and stay active. Her NHS GP suggests painkillers and a 12-week wait for a physiotherapy referral.
- The PMI Pathway: Sarah has a PMI policy with good out-patient and therapies cover. She uses the 24/7 GP service and gets an immediate referral to a private orthopaedic specialist. She sees the consultant four days later. The consultant suspects a disc issue and refers her for an urgent MRI, which she has the next day. The scan confirms a bulging disc.
- The Outcome: Her policy covers a course of six one-on-one sessions with a top physiotherapist, starting that week. The physio gives her targeted exercises that resolve the sciatica within a month. The swift diagnosis and treatment prevent chronic pain and allow her to get back to the gym, helping her on her weight loss journey. The total time from first call to treatment starting was less than one week.
Case Study 2: Mark, 52, Sales Director
- The Situation: Mark has a BMI of 31 (obese). He feels generally fine but is worried about his family history of heart disease. He knows it could take months to get a preventative health check-up on the NHS.
- The PMI Pathway: Mark’s policy includes a comprehensive annual health check as a wellness benefit. He books one at a private hospital. The results are concerning: his blood pressure is elevated, and his cholesterol is high.
- The Outcome: The private GP at the screening immediately refers him to a cardiologist under his policy. He sees the consultant within days. The cardiologist arranges an ECG and further blood tests, which confirm he is at high risk but hasn't had a cardiac event. The policy also provides a consultation with a dietitian. Armed with a clear medical picture and expert dietary advice, Mark makes significant lifestyle changes. He uses his policy's gym discount to start a fitness regime. A year later, his blood pressure and cholesterol are back in the normal range. He has successfully averted a potential heart attack.
Taking Control of Your Health Narrative
The UK's obesity crisis is a formidable challenge, both for the nation and for individuals. The statistics are not just numbers; they are a call to action. A reactive approach, waiting for the inevitable consequences of this disease time bomb to strike, is a strategy fraught with risk, delay, and uncertainty.
But there is a proactive path forward.
Private Medical Insurance, when understood and utilised correctly, is one of the most powerful tools at your disposal. It is your partner in prevention, providing rapid access to the diagnostics that can catch problems early. It is your coach for well-being, offering the resources and rewards to help you build a healthier lifestyle. And it is your safety net for treatment, ensuring that should a new, acute condition arise, you will receive the best possible care without delay.
It is not a magic wand for past health issues. It is a strategic investment in your future.
Taking that first step—acknowledging the risks and exploring your options—is the most crucial part of the journey. By considering how private healthcare can complement the NHS, you are not just buying an insurance policy; you are taking decisive control of your health narrative.
If you are ready to explore how a tailored private medical insurance plan can support your proactive health journey, our team of experts at WeCovr is here to help. We provide free, impartial advice to help you navigate the market and build a plan that protects your most valuable asset: your health.
Sources
- NHS England: Waiting times and referral-to-treatment statistics.
- Office for National Statistics (ONS): Health, mortality, and workforce data.
- NICE: Clinical guidance and technology appraisals.
- Care Quality Commission (CQC): Provider quality and inspection reports.
- UK Health Security Agency (UKHSA): Public health surveillance reports.
- Association of British Insurers (ABI): Health and protection market publications.